All published articles of this journal are available on ScienceDirect.
Peak Expiratory Flow Rate: A Useful Tool for Early Detection of Airway Obstruction in School Children
Abstract
Context:
Peak expiratory flow rate (PEFR) is an effort-dependent parameter, emerging from the large airways within about 100-120 msec of the start of forced expiration. It measures the degree of obstruction in the airways. A child from an asthmatic family, having significantly low PEFR values than its height and age matched peers, can be considered under impending asthma category.
Aims:
The present study was proposed to detect early stages of airway obstruction in school going children.
Settings and Design:
Observational study conceived in the department of Physiology, AIIMS, Jodhpur, Rajasthan.
Methods and Material:
Hundred students of age group 7-15 years participated in the study. A family history for presence/absence of asthmatic symptoms was taken from all subjects. After anthropometric examination, PEFR values were recorded in standing position, using the Mini Wright Peak Flow meter after demonstrating them the right procedure. Three measurements were taken and the highest reading was recorded.
Statistical Analysis Used:
Fisher’s exact test was done to calculate the two tailed ‘P’ value, Odd’s ratio and relative risk.
Results:
Thirty-one Percent children with family history of airway obstruction showed PEFR values below 80% of the predicted value, while 5.74% who were not having any family history of asthma, also showed values below 80% of the predicted value. With Fisher’s exact test, the two tailed ‘P’ value was 0.0155 (significant).
Conclusion:
The results of this study support the vital role of PEFR related to changes in airflow, which eventually can result in early identification of children with airway obstruction.
INTRODUCTION
The peak expiratory flow rate (PEFR) is a person's maximum speed of expiration. A subjective and effort-dependent parameter emerging from the large airways within about 100-120 msec of the start of forced expiration remaining at its peak for 10 msec, it varies with anthropometric, climatic, geographic and nutritional conditions [1-4]. It is measured with a peak flow meter, which is a simple, portable, hand-held device used to monitor a person's ability to expire out air through the bronchi. It thus gives an idea about the degree of obstruction in the airways.
Asthma, one of the most common chronic diseases of childhood, is characterized by recurrent, reversible, airway obstruction occurring usually because of inflammation of the pulmonary airways and bronchial hyperresponsiveness with eosinophilic infiltration [5]. Physiologically, abnormal airway hyper-reactivity is documented by decreased bronchial airflow after broncho-provocation with methacholine or histamine. Airway obstruction can also be provoked by cold air, exercise, viral upper respiratory infection, cigarette smoke, and respiratory allergens [6].
The global prevalence of asthma is anticipated to be approximately 4.5 percent [7]. In India, the prevalence of asthma in adults varies from 2.05 to 3.5% (17-30 million patients) [8]. Severe socio-economic burden is experienced by the family of asthmatics [9], the estimated total cost of asthma treatment for the year 2016 is calculated to be approximately 4852.86 crores [10]. Asthma is seen running in families not only because of the genetic inheritance but due to same exposures and environmental conditions shared by them.
Peak flow meter can serve as a useful tool to monitor airway patency particularly in those children who have a family history of bronchial asthma. A child from an asthmatic family, having significantly low PEFR values than its height and age matched peers, can be considered under impending asthma category.
Thus, present study was proposed to detect early stages of airway obstruction through PEFR, in asymptomatic school going children and to refer the subjects showing signs of early obstruction, for further pulmonary evaluation.
SUBJECTS AND METHODS
After obtaining the approval from the ethical committee of the institute, the study was conducted on school children in Jodhpur district, during their school hours. Prior permission from the school authorities and informed written consent from the parents/guardians of all children were obtained on a consent form, after clearly explaining them the purpose of the study.
Exclusion criteria were; any thoracic skeletal abnormality e.g. kyphosis, scoliosis, history of pulmonary surgery, malnutrition, acute respiratory infection or any medication with bronchodilators. Those with present or past history of smoking, pulmonary tuberculosis, COPD, bronchiectasis or any other respiratory diseases were also excluded from the study.
Hundred students, of age group 7-15 years were recruited for the study; of which 40 were girls and 60 boys.
Anthropometric parameters were measured. For all subjects, age was calculated to the nearest completed year. Weight (in kg) was measured without shoes and with light clothing, on a standard calibrated bathroom scale. Height (in cm) was measured with a standard portable stadiometer.
A personal and family history for presence/absence of asthmatic symptoms like shortness of breath, wheezing, cough, heaviness of chest and night time exacerbations of symptoms and/or any prolonged medication [11] was taken from all subjects. The children with any of these symptoms were not included in the study. However, such symptoms in any other family member suggested a positive family history. In those who gave a positive family history of asthma, the relation with the asthmatic family member, was also recorded. PEFR values were then recorded in standing position, using the Mini Wright Peak Flow meter. The maneuver was explained and demonstrated to them before the actual recording. Each child was asked to take a deep breath and then blow into the peak flow meter as hard and as quickly as possible. The peak flow meter was horizontally held and a tight seal was maintained between the lips and the mouthpiece. The marker was returned to zero after every measurement. A few normal breaths were taken and then the process was repeated two more times. Every child was encouraged to blow harder each time. Three measurements were taken and the highest reading was recorded on case record forms. Disposable mouthpieces were used for the subjects.
PEFR values were classified into 3 regions as described below:
- Eighty to 100 percent of the usual or normal peak flow readings indicated no airway narrowing.
- Fifty to 79 percent of the usual or normal peak flow readings were considered as mild airway narrowing.
- Less than 50 percent of the usual or normal peak flow readings indicated moderate/severe narrowing.
RESULTS
The study was performed on 100 asymptomatic children of age group 7-15 yrs, 40 girls and 60 boys. The mean age of males was 11.15 ± 2.3 years while that of females was 11.17 ± 2.6 yrs. Average height and weight of males was 142.7±12.67 cm & 35.94± 9.89 kg, respectively while that of females was 142.4 ± 14.82 cm and 38.47 ± 12.44 kg, respectively. The mean PEFR values in L/min were 281 ± 67.19 in males and 245 ± 39.06 in females. Descriptive analysis of PEFR was performed to calculate mean and standard deviation. PEFR value was the dependent variable while age, sex, height, and weight were the independent variables. The predicted values were obtained by using the following formulae [12].
Females: (3.92*Ht.)-277.01
Males: (4.08*Ht.)- 284.55.
The predicted value so obtained were compared with the observed values of PEFR. We found that the observed PEFR value of 91 students was above 80% of the predicted value (no obstruction in airways) while 9 children had observed PEFR values below 80% of the predicted value (suggestive of narrowing of airways). Of these, 4 had PEFR values more than 75%of the predicted value; 3 had values between 65%-75% of the predicted values and 2 had PEFR values below 65% of the predicted value. The lowest observed PEFR was 56.2% of the predicted value.
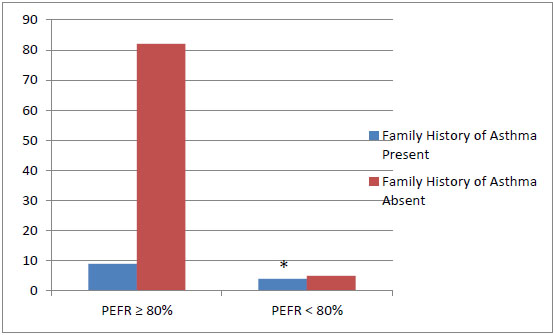
Thirteen percent children gave a family history of asthma. Four out of 13 children (30.76%) with family history of airway obstruction showed PEFR values below 80% of the predicted value. On the other hand, five children (5.74%) who were not having any family history of asthma, also showed values below 80% of the predicted value. Surprisingly, the child with lowest PEFR value 56.2% of the predicted value had no family history of airway obstruction (Fig. 1). On applying Fisher’s exact test, the two tailed ‘P’ value was 0.0155 (significant). Relative risk was 0.7345 and Odd’s ratio came out to be 0.1372.
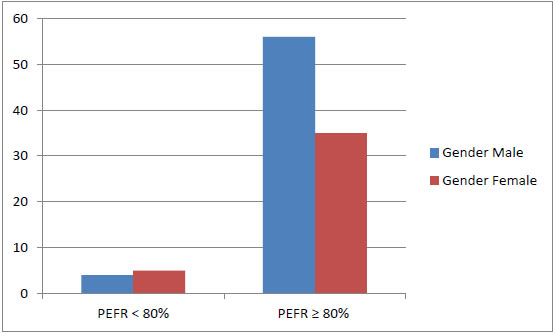
We tried to explore the gender differences in PEFR values in our cohort (Fig. 2). On applying Fisher’s exact test, the two tailed ‘P’ value was 0.4776 (not significant). Relative risk was 0.7222 and Odd’s ratio came out to be 0.5000.
The variations of PEFR with respect to the socioeconomic status of the children has been shown in Table 1.
| Socio-economic status | Total | |||
|---|---|---|---|---|
| High | Middle | Low | ||
| PEFR ≥ 80% | 9 | 74 | 8 | 91 |
| PEFR ≤ 80% | 0 | 8 | 1 | 9 |
| Total | 9 | 82 | 9 | 100 |
The children with low PEFR were thus identified and the school authorities were told about them. They were advised for further pulmonary evaluation.
DISCUSSION
In this pilot study, we estimated PEFR in asymptomatic school going children, with an aim to detect whether children with positive family history of asthma are at an increased risk of developing asthma later in life. Since PEF testing has good screening properties to detect airway obstruction, we can identify children with airway obstruction in the pre-clinical asymptomatic stage and preventive measures can be instituted before the frank development of disease. Various studies have been done on PEFR in the past. In 2002, Rajesh Sharma et al. studied PEFR in a group of rural school going children, from Ajmer district of Rajasthan state and compared the values with those available from Northern India [13]. Lee HS and others suggested PEFR to be a useful additional tool to the respiratory questionnaire and spirometry in asthma cases, as it measures airway variability [14-16].
A few studies have attempted to compare the PEFR values of highlander and lowlander populations and found a significant rise in PEFR among high-altitude residents [17]. A number of studies have distinctly substantiated the effect of various anthropometric parameters like age, height, and weight on lung function in normal children [18-20].
In 2013, Manjunath CB et al. felt that since the reference values of PEFR were affected by regional, environmental and anthropometric factors, hence it was necessary to have regional reference values for children. Thus, they studied PEFR in 1028 children aged 5 to 16 years by using Wright’s mini peak flow meter and found that among different factors affecting PEFR, height correlates better with PEFR than weight and sex [21]. In 2013, Mishra et al. also found that height correlates better with PEFR in males and weight correlates better with PEFR in females [22]. Paramesh H. found that PEFR values correlated best with height, there was no difference in sexes, religion and urban/rural children [23]. Various researchers have concluded that the highest correlation of PEFR occurs with height and they constructed nomograms relating PEFR to height [12, 24-26].
Since most of the studies have proved that height is the most effective variable affecting PEFR, we used a prediction equation based on height, given by Swaminathan et al., for predicting the PEFR values of our group of subjects [12]. The results of our study suggest that children with positive history of asthma are more prone to develop airway obstruction. In our study 30.76% children with family history of airway obstruction showed PEFR values lower than their matched peers. Our study is supported by Burke et al. who assessed the predictive value of family history as an indicator of risk for childhood asthma [4]. It is a well-known fact that asthma runs in families. Evidences suggest that this high familial association occurs not only because they share genetic makeup, but also the same environmental factors play an important role in asthma etiology. The association of a positive family history of asthma along with a decreased PEFR to identify children at increased risk, could provide a basis for targeted prevention efforts.
The results of this study support the pivotal role of PEFR aimed at providing data related to changes in airflow, which eventually can result in early identification of children with airway obstruction, timely intervention and medication to improve symptom control. When asthma symptoms are controlled, children are less restricted in their ability to participate in various activities and experience less emotional distress. With the alleviation of asthma symptoms, children’s Quality of Life (QOL) scores will improve [27, 28]
We conclude that PEFR, which is regarded as an early determinant of airway obstruction even in asymptomatic states, is a very simple procedure that does not require any specialized, sophisticated instrument or assistance; it could be performed routinely, may be biannually, in schools as a screening procedure to detect early airway narrowing particularly in children with a positive family history of asthma.
The limitation of our study is its small sample size, we suggest that this study should be conducted on a larger sample to increase the power of the study. Although proper instructions were given and all the recordings were done by the same technician throughout the study, the chances of getting false positive results could not be denied as the PEFR is effort-dependent. Study correlating PEFR with various spirometric parameters can be planned to identify false positive cases. Further, we can correlate PEFR values with another easily performed lung function test i.e. SpO2/MHR index.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Indian Council of Medical Research for supporting the study through its Short term Studentship programme.


