All published articles of this journal are available on ScienceDirect.
A Pilot Programme for Tuberculosis Screening in Immigrants at Primary Care
Abstract
Background:
Immigrants from countries with a high prevalence of Tuberculosis (TB) may constitute a source of infection.
Objective:
The aim of the present study was to describe a Tuberculosis (TB) screening programme at a primary health care centre directed at immigrants from countries with a high prevalence of TB.
Methods:
This was a descriptive study conducted at a primary health centre in Barcelona between 2009 and 2012 for immigrants from countries with a TB incidence > 100/100,000. They were invited to join the TB detection programme on registering at the primary health care centre when a reference nurse conducted a survey on socio-health data, performed a Tuberculin Skin Test (TST) and requested a chest X-ray. Interferon Gamma Release Assays (IGRA) were applied in individuals with positive TST or an abnormal X-ray.
Results:
Ninety-one (70.5%) of 129 individuals, aged 29.8 ± 9.8 years, who entered the programme, were men, 60 (46.5%) were from Pakistan and 3 reported previous TB. Eighty-six (66.7%) immigrants completed the study protocol. Three cases (2.3%) of TB were diagnosed and 29 (30.5%) had latent TB infection. Seven chest X-rays yielded other non-TB radiological changes.
Conclusion:
This TB screening programme should aid early detection of TB and LTBI among immigrants from high-TB prevalence countries on first registering at the primary health care centre.
1. INTRODUCTION
A decrease in the overall rate of Tuberculosis (TB) has been reported in the countries of the European Union and the European Economic Area in the last 15 years. However, the number of cases among immigrant populations, particularly those from high-TB prevalence countries, has been gradually increasing, thereby contributing significantly to maintaining the burden of disease [1]. In some countries such as the UK, Sweden and the Netherlands, cases among immigrants account for over 50% of all TB cases [2]. Furthermore, the new immigration wave occurring in Europe suggests this trend may continue to grow in the coming years.
It is paramount to ascertain whether new cases of TB among immigrants are due to reactivation of a Latent TB Infection (LTBI) acquired in their country of origin or to disease acquired after their arrival in a new country to establish TB control strategies. Clinical evidence suggests that a significant rate of TB among immigrants developed from an infection acquired in their country of origin [3, 4]. The fact that the country of origin can accurately predict the number of cases that will arise later together with the number of cases from which an immigrant could be identified as at risk, are additional challenges [5]. There is a long-standing demand to develop strategies for the early detection of TB and LTBI among immigrants from countries with a high-TB prevalence to prevent progression of the disease [6].
Primary health care has been identified as key in controlling TB among immigrants [7]; however, clinical evidence showed that TB screening is not routinely performed in this setting [8] nor will it usually follow the national guidelines [9]. In Spain, it is recommended that all immigrants be given a health card and be medically screened at first contact with the health system [10]. Following this recommendation, a TB screening programme was launched at a primary health centre for immigrants from high-prevalence countries. The programme attempted not only to detect TB cases but also LTBI, which is considered crucial to prevent progression of the disease [11]. The aim of the present descriptive study was to explore this TB screening programme at a primary health centre.
2. METHODS
The programme was aimed at immigrants from countries most affected by TB (incidence > 100/100,000) and established with the Public Health Agency of Barcelona, according to the Guidelines for the Prevention and Control of Tuberculosis in Barcelona and the WHO recommendations [12, 13]. The study protocol was approved by the local Ethics Committee and all participants were individually assessed according to their cultural and social background to ensure equity among participants and signed their informed consent [14].
The programme was carried out from March 2009 to March 2012 at the primary health centre of Barceloneta. This area covers Ciutat Vella, the inner-city district of Barcelona with a population of around 15,000 inhabitants with a high ageing population and many reduced-space homes (around 40 m2). Approximately 5,500 of the population in this district was born abroad, a higher rate than the city average according to the 2014 municipal census [15].
2.1. Screening protocol
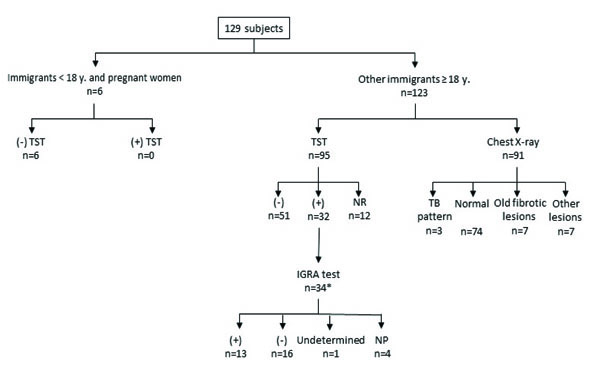
The study protocol for TB screening in the immigrant population treated at the Barceloneta primary health centre is shown in Fig. (1). When there was a language barrier, the centre had an interpreter available. Briefly, at the time of their first registration in the health centre, immigrants from risk countries were invited to join the TB detection programme. Booklets with information in different languages were available, and participants gave their written informed consent, after which they were promptly directed to a reference nurse (5-15 minutes) who conducted a survey regarding epidemiological, clinical and demographic data such as previous diseases, alcohol abuse (yes/no), smoking (yes/no), other toxic habits (heroin, cocaine, cannabis and benzodiazepine consumption), financial vulnerability according to the need for social resources (yes/no), precarious employment (yes/no) and previous TB or therapy for LTBI. BCG vaccination status was not considered. Next, the nurse performed the Tuberculin Skin Test (TST) using 2 units of PPD-RT 23 with Tween 80, made an appointment for test reading three days later and requested a chest X-ray at the radiology department of the Hospital del Mar (located next to the primary care centre). This form identified the subject as a participant in the programme, and that he/she underwent a chest X-ray shortly after arrival (usually between 10 and 60 minutes). All chest X-rays were reported by specialists and sent to the referring GP.

The TST was considered positive if induration was ≥ 10 mm. In patients with immunosuppression, radiological images of previous fibrosis, recent TB contacts, or symptoms suggestive of TB, the limit was 5 mm. All patients with abnormal chest X-ray or positive TST were referred to the GP.
For asymptomatic subjects with a normal chest X-ray and positive TST, or radiological pattern suggestive of TB with negative/not performed TST, Quantiferon TB Gold in Tube [16] was performed. This Interferon-Gamma Release Assay (IGRA) has been approved for the in vitro quantification of the cellular immune response using antigens specific to Mycobacterium tuberculosis. In the same blood test, routine biochemical analyses, serologies for Human Immunodeficiency Virus Infection (HIV) and hepatitis virus were determined.
The results of these tests were subsequently evaluated and, if necessary, other complementary examinations and the need for therapy for TB or LTBI were also evaluated. TB diagnosis was based on clinical data plus the TST, chest X-ray and IGRA test. In all cases, the diagnosis was confirmed through Löwenstein culture.
In general, treatment for LTBI was started when TST and IGRA were positive. However, each case was individualised depending on the clinical characteristics of the patient, the probability of adherence to LTBI treatment, and age (priority to those < 35).
2.2. Statistical analysis
Data were expressed as mean ± Standard Deviation for continuous variables (age) and as percentages and frequencies for categorical variables (sex, nationality, smoking, alcohol consumption, other toxic habits, financial vulnerability, known liver disease, previous TB or previous positive TST). Student's t-test was performed to assess differences between two means. Chi-square or Fisher’s exact tests were used to evaluate the degree of association of categorical variables.
All statistical analyses of database results were made by the Statistical Package for the Social Sciences (SPSS for Windows v. 12).
3. RESULTS
The main clinical characteristics of the 129 subjects who joined the programme are shown in Table 1. Pakistani nationality was the largest (46.5%), followed by Nepalese (11.6%) and Indians (9.3%). TB and LTBI patients (n= 32) had higher alcohol (43.8% vs. 10.6%; p <0.006) and smoking (25.0% vs. 4.5%; p <0.005) rates than the other screened subjects.
TST was read in 83 of the 129 participants (64.3%): 51 were negative (61.6%) and 32 positive (38.6%). Of the remaining 46 cases, 12 failed to return for test reading and 34 did not attend the TST (Fig. 2).
Chest X-ray was indicated in 123 participants and taken in 91 (74%) and was not indicated in 6 cases (5 teenagers and 1 possible pregnancy) (Fig. 2). The 32 participants, who did not have the chest X-ray indicated according to the protocol, did not attend the radiology clinic to have this performed. Of the 91 chest X-rays performed, radiological lesions consistent with TB were observed in three cases, while seven chest X-rays revealed old fibrotic TB lesions (Fig. 2); a further seven chest-X-rays demonstrated other non-TB radiological changes including azygos lobe, pericardial effusion and Poland syndrome.
The IGRA was carried out in 34 patients including two of the participants with radiological changes consistent with TB who did not have a TST performed. The IGRA was positive in 13 cases (38.2%), 11 of whom were diagnosed with LTBI and two were diagnosed with TB in this study.
3.1. Cases of TB and LTBI
Three cases (2.3%) of TB, cervical lymphadenitis, pulmonary cavitary lesion and interstitial lung pattern, all in patients of Pakistani origin, were detected among the 129 participants in the programme; however, if we consider only subjects with a chest X-ray taken (91 cases), a 3.2% prevalence of TB was found. A fourth participant had a chest X-ray characteristic of TB, although the follow-up to confirm this diagnosis was not possible.
LTBI was diagnosed in 29 subjects with positive TST (excluding three TB cases), which represents 30.5% of all TST read. Eight of 15 Nepalese (53.3%) and 8 of 60 Pakistanis (13.3%) were diagnosed as LTBI. Mean age of patients with TB or LTBI (35.5 years) was slightly higher compared with the remaining patients (28.4 years). All LTBI patients, with positive TST and IGRA (n=13), who were considered for a regimen with isoniazid and rifampin daily for three months, completed the treatment.
During follow-up, two cases of chronic hepatitis C, one of cardiomyopathy and one of hypertension, were also diagnosed.
4. DISCUSSION
Population mobility across the world is rapidly becoming a key determinant of infectious disease epidemiology. The relationship between migration and TB control has been extensively addressed [17]. Immigrants have an increased risk for TB, depending on the TB incidence in their country of origin, conditions of their migration and duration of stay in the host country. In Spain, according to the National Epidemiological Surveillance Network [18], the incidence of TB in 2015 was 10.59 cases per 100,000 inhabitants, with the percentage of subjects born in other countries being approximately 30% of the total. We must take into account that this percentage varied greatly among the different autonomous communities, with Catalonia and Madrid having the highest percentages (37 and 20%, respectively). In the present study, of 129 immigrants from high-TB prevalence countries who entered the programme at a primary care centre, 3 (2.3%) new cases of TB and 29 (30.5%) of LTBI were detected. These results are close to those published in a systematic review and meta-analysis to determine the performance of screening in detecting active TB at the point of entry [19] and provide useful data for the development of rational services for active detection of TB in immigrants, especially at primary health centres. Therefore, these findings support the fact that in low-TB incidence countries, systematic screening of immigrants at high risk for TB may be considered a key intervention in progress towards TB elimination [20].
| Variables | Value |
|---|---|
| Age, years (mean ± SD) | 29.8 ± 9.8 |
| Gender, men (%) | 91 (70.5) |
| Smoking, n (%) | 18 (14.0) |
| Alcohol consumption (≥ 2 units), n (%) | 9 (7.0) |
| Other toxic habits*, n (%) | 3 (2.3) |
| Financial vulnerability, n (%) | 59 (68.2) |
| Known liver disease, n (%) | 6 (4.7) |
| Previous tuberculosis, n (%) | 3 (2.3) |
| Previous positive TST, n (%) | 1 (0.8) |
Times for screening for infectious diseases vary from country to country: either prior to arrival, on arrival or later [21]. Detection strategies for newcomers at the time of arrival have been successful in countries such as the United States [22], with a significant reduction in the number of TB cases [23]. However, there have been few reports on TB screening in the primary health care setting. It is therefore difficult to compare the present results with reports from other similar settings. Several studies have demonstrated that the costs of the early detection of TB and LTBI outweigh those of subsequent TB treatment [24]. This supports the need for new strategies designed to increase access to TB screening, particularly for high-risk populations such as immigrant communities.
The programme demonstrated a remarkable fulfillment rate compared with other experiences in detecting TB in immigrants [25]. The presence of responsible staff in all areas involved in the programme, very clear algorithms, and prompt completion of tests may explain this high participation. Furthermore, the proximity of the primary care centre and hospital radiology department could explain the high rate of chest X-rays performed in the present study, slightly higher than the TST. Nevertheless, 34 patients did not have a chest X-ray.
The distribution of TB cases and LTBI by country was similar to that reported in 2014 in relation to the detection of TB prior to entry into the United Kingdom by the National Health Service [26]. Therefore, these programmes make sense, particularly in countries where no screening is performed on arrival. In the present study, the detection of 29 (30.5%) LTBI cases is highly relevant, since 5-10% of these cases will develop active TB, and the risk rises substantially in smokers (2.5 times) and those with HIV infection (10 times) [27].
The IGRA technique is more specific and, in some studies, more sensitive than TST [28]. The combined use of TST and IGRA is already recommended in various guidelines and specifically in healthy individuals who have a low risk of progression to TB [29]. Positivity of the IGRA technique predicts the long-term development of TB compared with positive TST [30]. Thus, considering the use of TST and IGRA techniques together, as in the present study, can be a good strategy for deciding to start therapy for LTBI in this risk group [31].
Some limitations should be noted. Unfortunately, we cannot accurately calculate the total population invited to enter the programme. However, during the study period, 802 immigrants from risk countries were registered at the primary health centre. If health institutions emphasised its importance, it would become a similar procedure to others already conducted in welcoming new patients and should not be considered a difficulty that cannot be overcome.
CONCLUSION
The present findings support an active TB search in immigrants from high-TB prevalence countries at the time of their registration at the primary health care centre, mainly when immigrants are not screened on arrival. Screening programmes targeting high-TB risk groups within the framework of coordinated activities of TB management can successfully improve the control of the disease. Furthermore, the early detection and management of TB among immigrants are expected to prevent unnecessary transmission.
LIST OF ABBREVIATIONS
| TB | = Tuberculosis |
| TST | = Tuberculin Skin Test |
| IGRA | = Interferon Gamma Release Assays |
| LTBI | = Latent TB Infection |
| HIV | = Human Immunodeficiency Virus Infection |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by the local Ethics Committee.
HUMAN AND ANIMAL RIGHTS
No animals were used for this study. All humans research procedures performed in the current study were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki declaration of 1975 as revised in 2013.
CONSENT FOR PUBLICATION
All participants were individually assessed according to their cultural and social background to ensure equity among participants and signed their informed consent.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise
ACKNOWLEDGEMENTS
We thank Miss Christine O’Hara for review of the English version of the manuscript.


