Diverticulization Duodenal Distal Technique for Injury Angle Duodenojejunal
Abstract
Duodenojejunal injuries region at the angle of Treitz are rare, variable etiology and often associated with other serious injuries. In trauma situations with perforations and bleeding, his approach is often difficult. The primary suture, resection / anastomosis and duodenal exclusion are the usual for trauma management techniques in this region. The aim of this paper is to show the initial results of an alternative for injuries duodenojejunal angle (IDJA) by filling a retrospective, descriptive and observational technique, 12 patients operated were analyzed over a period of 15 years, carriers IDJA, age: 34, 11 gunshot wound. 92% of the cases had other associated visceral injuries. The average for the ISS was 29. In all cases located in duodenum duodenojejunoanastomosis II, via the right lateromesenterica upon closing section and duodenum level III was performed. 58% of cases were complicated. Mortality case series were 1 (8%) digestive suture failure colon. Average Hospital stay 26 days.
Conclusion:
A simple, safe and maintaining gut physiology is proposed technique; with a single anastomosis, located in well-vascularized area and away from bruising and contaminated areas. The complications were pancreatic fistula and digestive suture failure.
INTRODUCTION
Injury duodenal jejunal angle are rare (15% of all duodenal lesions) usually associated with trauma and complex for associated injuries. The primary suture, resection/anastomosis and duodenal exclusion techniques are commonly used for its simplicity and relative safety; while leaving a digestive suture located in a section of the digestive tract of low and variable vascularization as the angle of Treitz with results showing up to 25% mortality and complications between 30-60% [1].
In a previous publication the technique of distal duodenal diverticulizacion, benefits and an initial experience of three cases described [2].
The aim of this study is to report our recent experience in the surgical management of IDJA.
METHODS
It was a retrospective, descriptive and analytical study of a series of 12 cases operated in the Maciel Hospital of Montevideo (Uruguay) in a 15-year period (January 1998 to December 2013). The database and statistical analysis was performed with SPSS 19 for Windows.
Was considered statistically significant p <0.05.
Qualitative variables are expressed as a percentage, while quantitative using the mean and standard deviation (SD).
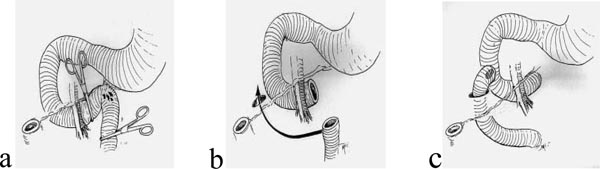
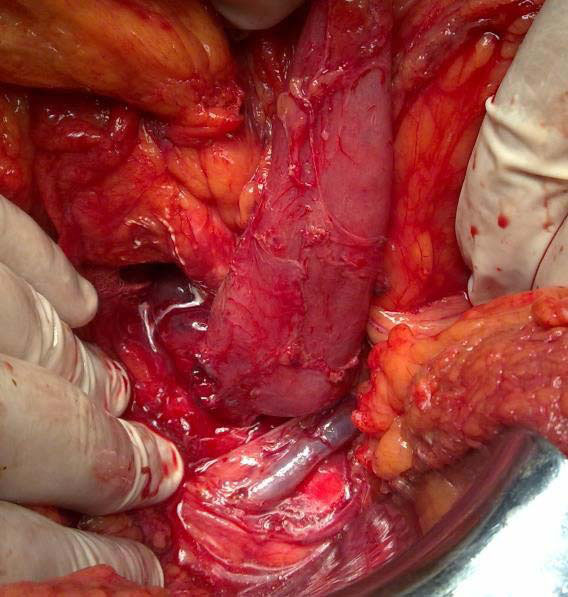
The surgical technique used for the management of all patients consists of 3 steps: a) Mobilization of angle duodenal jejunal resection and closure of duodenal III / IV. b) Passage out latero via jejunal mesenteric right through the avascular area of the transverse mesocolon. c) Preparation of duodenal jejunal anastomosis located on duodenum II Figs. (1-3).
In all cases it was placed prophylactic drainage.

RESULTS
In the analyzed period 12 wounds in the region of the angle of Treitz, including 11 by gunshot wound and a perforation through the ingestion of a foreign body (matt bulb) were recorded. All patients were male; age 34 years ± 11 years.
Most cases (92%) had associated lesions: 4 pancreas, 2 colon, 2 spleen, stomach 2, one liver, mean ISS 29. In all cases the angle jejunal resection was performed duodenum, followed located in a duodenum duodenojejunoanastomosis II, as was described previously.
Duodenal lesions were 1 case grade II, grade III 8 cases and 3 grade IV classification AASTOIS [3].
Complications occurred in 58% of cases: 3 pancreatic fistulas, 1 fails colon suture 1 paracolostómico abscess and duodenal suture failure attributable to this technique.
In any case there was leaks in duodenal III.
Mortality 8%: gastrointestinal suture failure colonica. Average Hospital stay 26 days (Table 1). A statistically significant difference (p = 0.006) of major complications in patients with associated lesions were observed.
| Complications | 58% | Pancreatic fistula | 3 |
| Fail suture colon | 2 | ||
| Fail suture duodenal II | 1 | ||
| Pericolostomic abscess | 1 | ||
| Bleeding | 1 | ||
| Mortality | 8% | Fail suture colon | |
| Hospital stay | 26 days |
DISCUSSION
The duodenojejunal region and the angle of Treitz is located deep in the abdominal cavity; vascularization is variable, relatively unstable and has close relationships with vascular anatomical structures and vital organs. Therefore, although the wounds that level are exceptional resolution even constitutes a technical and tactical challenge.
Should be understood IDJA usually are complex and serious, because mostly associated with other injuries that affect the primary patient management. Surgical tactics must be within the meaning of damage control, prevent complications (sepsis, pancreatic fistula) and the surgical technique will reflect the severity of the injury.
Of the multiple procedures in the literature [4] (Table 2), primary duodenal repair (duodenorrhaphy) is the most common surgical technique for simple traumatic injuries of the duodenum (grade I and II). Faced with complex lesions (grade III and IV) to duodenorrhaphy you can add pyloric exclusion as proximal duodenal bypass technique.
| Duodenorrhaphy. |
| Duodenorrhaphy with duodenostomy tube. |
| Ostomy triple technique (gastrostomy, and jejunostomy duodenostomy) |
| Jejunal serosal patch |
| Duodenal Diverticulizacion |
| Pyloric exclusion |
| Duodenopancreatectomy |
The duodenal exclusion is widely described and tested at the level of the proximal parts of the duodenum (I-II) [5-8], technical results while managing injuries fourth portion, Carrillo [9] proposed debridement or resection with primary anastomosis -duodenal duodenum, the duodenal Cogbill [10] used for resection anastomosis and Nassoura [11] type III lesions the same procedure for the most duodenal lesions. Still it is clear that the sutures are placed throughout an environment of hemorrhage and contamination.
This short series of cases shows the management of grade III-IV lesions located at the level of the fourth portion of the duodenum and the results obtained with the proposed technique(mortality 8% morbidity 58%) are comparable to literature whose disease is 46% and 14% mortality.
Morbidity should be analyzed considering that there is a high incidence of complications in patients with higher number of associated injuries (p <0.05).
The proposed technique has the benefit of being: a) physiological, because it keeps the duodenoyeyunal continuity; b) avoids leaving a contaminated environment anastomosis; allows a suture without tension and ends well vascularized and is simple, reproducible and easy to apply.
It must be admitted that the main difficulty of this technique is that it requires extensive mobilization of duodenal jejunal angle, which can be difficult in terms of bleeding or instability of the patient; but in this circumstance is essential exploration of it to avoid inadvertent injury, even as part of a tactical damage control.
CONCLUSION
The IDJA are exceptional, complex and difficult to establish a common tactic.
A tactical resource, safe, simple and feasible in very acceptable results is described. Associated injuries were instrumental in the presence of developmental complications. The failure of gastrointestinal and pancreatic fistula suture were the most frequent complications.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


