All published articles of this journal are available on ScienceDirect.
The Deconstruction of a Complex Case of Medical Child Abuse
Abstract
Background:
Medical child abuse (MCA) is a serious and potentially fatal form of child abuse. The condition of medical child abuse has historically been regarded as a “rare” entity. However, the lack of a standardized definition of medical child abuse may have limited our understanding of the true scope of the problem. Cases may straddle the elements of physical abuse, medical neglect, and psychological abuse. Many cases may have been overlooked as medical child abuse or categorized under another form of child maltreatment, when identified as abuse or neglect. There is no one typical presentation. Medical investigations into suspected cases must be carefully and conservatively conducted.
Method and Result:
An illustrative case is described involving three young chronically-ill siblings with various degrees of medical dependencies, medical and surgical interventions, and multiple subspecialists and is deconstructed with the final outcome of three physically healthy children and a criminal conviction of the perpetrating caregiver.
Conclusion:
Cases of child medical abuse can be complex and challenging. Potential complications and sequelae of unidentified cases are vast, including: pain and suffering from multiple, unnecessary procedures, diminished quality of life and life potential, and ultimately risk of death. Challenges to medical and social investigations can hinder early identification and protection of the children at risk.
INTRODUCTION
Medical child abuse (MCA), formerly Munchausen syndrome by proxy (MSBP), is a serious and potentially fatal form of child abuse [1] Since its initial description as Munchausen Syndrome by Proxy [2], this particular form of child maltreatment has been described over the years by many proposed and controversial nomenclatures, including pediatric condition falsification [3], child abuse in a medical setting [4], medical child abuse, and caregiver-fabricated illness in a child [5]. The terms medical child abuse and caregiver-fabricated illness in a child attempt to bring the focus of the diagnosis back on the child patient as a victim. The diagnosis is made from the pediatric medicine vantage rather than an adult psychiatric purview as the determination of harm is directly made by the pediatric clinician regardless of the caregiver’s motivation or cause. The use of direct, clear terminology in the description of this form of child maltreatment is necessary when such cases transcend into the legal and criminal realms where clear understanding and communication of a complicated medical course are required for non-medical child protective and prosecutorial agencies. No matter the selected term, this is an unusual form of child maltreatment in which harm or potential harm is enacted onto the child through the use of the medical system at the instigation of the caregiver.
MEDICAL CHILD ABUSE
The condition of Medical child abuse has historically been regarded as a “rare” entity. However, the lack of a standardized definition of medical child abuse limits our understanding of the true scope of the problem. Such cases straddle the elements of physical abuse, medical neglect, and psychological abuse. Many cases may have been overlooked as medical child abuse or categorized under another form of child maltreatment, when identified as abuse or neglect. The diagnosis of MCA is often difficult and elusive, with an average time from onset of symptoms to diagnosis of 14.9 months (range 0-240 months) and 21.8 months (range 0-195 months) reported, respectively, in 2 large series [6, 7].
The following case of three siblings with medical histories of chronic, debilitating illnesses and dire prognoses underscores the need for early identification.
Case Study
The three children of a single, divorced woman, who was estranged from her own family, were well known to a small community in Texas. The children: “Charlie” (age 11), “Travis” (age 9), and “Heather” (age 6), were known to be medically-fragile children and were so ill that they were all home-schooled since Charlie began kindergarten. The children each suffered from multiple medical conditions requiring multiple doctor visits, which included several subspecialist visits. As the nearby metropolis housed a world-renowned medical center with multiple pediatric medical institutions, the seeking of second and third opinions from the varied and separate hospitals in the area was pursued as well.
Through the course of their young lives, these children carried sundry medical diagnoses and symptoms: global developmental delay, failure to thrive, seizure disorder, hypotonia, gastrointestinal malabsorption, gastro-esophageal reflux, urinary incontinence, stool incontinence, heat intolerance due to poor thermoregulation from a metabolic disease state, attention deficit/ hyperactivity disorder, Tourette’s syndrome, decreased acoustic reflexes in the right ear, obsessive-compulsive disorder, anxiety disorder, pragmatic language disorder, decreasing IQ scores, sensory integration disorder, auditory processing disorder, and poor immune function. Charlie and Heather were wheelchair bound, with Heather being able to walk only short distances with leg braces. Charlie and Heather were each fed via gastrostomy tubes and Charlie had a vagal nerve stimulator (VNS) surgically inserted for management of intractable seizures that were not controlled by medications.
The children were each on several different medications to be taken at various times of the day each day for psychiatric and medical reasons. They lived in a darkened home where thick drapes covered the windows given their complaints of photosensitivity to light. Due to their fragile state, they were very rarely allowed to go outside to shout and play in the sunshine. They did make random appearances in their community church, in their wheelchairs. The church held fundraisers and assisted in providing extra home care and travel needs that the mother required in her ongoing daily requirements in taking care of her 3 medically-fragile children. The pursuit for answers to the children’s many ailments, including a unifying diagnosis that would address all of the children’s symptoms, was constantly sought by the children’s mother. Ultimately, a presumed diagnosis of mitochondrial disorder was acknowledged by physicians caring for the children.
When the children’s mother fell ill and required hospitalization one summer, several church members volunteered in caring for the children during their mother’s absence. During that period of time which consisted of a few weeks, it was observed that when the children were properly fed and cared for, they began to gain weight and flourish. In one conversation Charlie had with one of the volunteers, the volunteer remarked with amazement that Charlie had had such an active day and that he didn’t appear to be tired or need his wheelchair, to which Charlie responded that he only uses his wheelchair in “big buildings, big buildings with doctors.”
Several calls to Child Protective Services (CPS) had been made over the course of several years regarding concerns for the welfare of the children by various members in the community. As the mother presented as a concerned, single, sympathetic mother with three medically-dependent children, the cases were quickly dismissed. The church members met with the same reactions from CPS when they attempted to report on what they were experiencing with the blossoming of the children in their short observation and interactions during the mother’s hospitalization. Not deterred, the ladies ultimately approached a law enforcement officer and voiced their concerns. The officer had never heard of “Munchausen syndrome by proxy”, but conducted a search on the internet and found the name of a local prosecutor who had recently convicted a mother of a fatal case of MSBP. With a convincing presentation and discussion regarding the quick apparent resolution of many of the symptoms by objective observations by non-medical, non-familial persons now involved in the care of the children, the prosecutor became concerned for the welfare of the children and the possible long-standing ruse created by a caregiver.
A new CPS referral was made given these concerns. Remarkably, even after having been informed of the new allegations from non-medical personnel, the CPS worker who visited the children in their home believed the mother and recommended the children be left with her. Only after the prosecutor and investigator called a meeting with CPS supervisors did the agency finally take action and place the children in the care of their maternal grandparents. The complicated medical regimen, copious medications, and numerous medical appointments for each child overwhelmed these new caregivers of the children. At this point, Children’s Protective Services requested the assistance of Texas Children’s Hospital to offer guidance and clarification of the true medical needs of the children.
Texas Children’s Hospital’s Child Abuse Pediatrics Team reviewed the case, and with the coordination of the Texas Children’s Hospital’s Critical Care team planned scheduled admissions that would allow each of the siblings to be observed on a monitored unit. During each child’s admission, a subspecialist from various medical disciplines from which the child carried an identified presumed diagnosis would then evaluate the child objectively without the possible historical distortion of a caregiver. With each physician’s evaluation, which included a review of the past medical record with previously performed diagnostic tests and results and very minimal but judicious subsequent testing, the previously presumed medical diagnoses were formally dismissed.
In less than a week of hospitalization, each child’s complicated medical regimen was significantly weaned to one or two drugs on discharge, and eventually to none. Each child who had a history of being unable to eat by mouth, was observed to tolerate oral feeds and subsequently underwent surgical removals of their gastrostomy tubes during this time period. A telling moment into the indoctrinated environment that the children lived in came when Heather was first fed orally, and a terrified Charlie screamed, “No! She can’t eat, she’ll die!” The hospital staff observed and documented how Heather relished in the various tastes and textures to which she was now introduced.
The three children who came into the hospital in wheelchairs, within the week of hospital monitoring, were observed by the medical and nursing staff to be racing through the halls of the ward and jumping on trampolines. All three children, who entered the halls of the hospital carrying over a dozen serious and potentially fatal diagnoses, left with a clean slate save for a diagnosis of reactive amblyopia given that they had been instructed to wear eyeglasses with thick lenses. As all of the serious medical diagnoses were dismissed, the final unifying diagnosis of medical child abuse was made. While this intervention and the ultimate diagnosis laid the foundation for the children to begin a more positive course for life, their journey was not without negative effects. The children who endured unnecessary medical and surgical procedures will continue with a lifetime of both emotional and visible scars of their childhood.
It is notable that a legion of physicians from different subspecialties and institutions interfaced with this family and each of the children, none of whom recognized that they were all victims of MCA at the hands of their mother. The young primary care physician, who had inherited this family from her partner years before, had even written a letter to CPS in support of the mother detailing the numerous medical ailments and requirements for each of the children when CPS removed them from her care and into the maternal grandparents’ home. After a month of the children’s therapeutic separation, realizing that each of the children’s true clinical picture was completely counter to what she had perceived as dictated by the mother, a subsequent letter was written remarking on her complete change of medical opinion. In part, the decisions made in previous CPS investigations were influenced by the physicians involved in the care of these children and the enormous number of treatments they were receiving. Why would the doctors be providing unnecessary treatment? And in this current investigation CPS received a letter from a physician stating that they were indeed “sick.”
It was discovered that over the course of the children’s lives, the family had traveled to Disneyworld through the “Make a Wish” Foundation, garnered over $150,000 in donations in the last couple of years before the rescue, and at the time of the mother’s criminal charge of injury to a child, was on the waiting list for “Extreme Home Makeover.” Today the two youngest children are thriving and excelling, enjoying family (now in the custody of their biological father) and friends, making the honor roll, and dancing in the sunshine. The oldest child, 11 year old Charlie, required continued mental health evaluations years later due to his protracted clinical course and numerous medical interventions over nearly most of his childhood, that were revealed to be largely unnecessary and superfluous.
DISCUSSION OF MEDICAL CHILD ABUSE
While medical child abuse has been considered an uncommon form of child abuse, the true prevalence of the condition is unknown given the lack of a clear and standardized definition. There is no one typical presentation for this form of abuse, although there are often commonalities in symptoms and diagnoses. In selected case series, the mortality rate has been defined as 6-9% (6) (7). The morbidity rate for cases is 100%. As in the spectrum of any disease, various gradations of fabrication and severity can be observed. A case may begin as one of relatively harmless exaggeration of symptoms and extreme hypochondria but over time evolve to deliberate and continual fabrication of symptoms, prompting medical investigations resulting in unnecessary medical or surgical procedures, and/or the more serious and potentially fatal induction of symptoms (i.e. intentional suffocation, poisoning).
When barriers or resistance from the medical establishment thwart the caregiver’s request for further medical interventions, other medical opinions are often persistently sought [8]. It is not unusual that these victims have been evaluated and treated at multiple medical institutions. Suspicions may be raised when the caregiver exaggerates or misrepresents normal observations, or when the historical features reported by the caregiver do not correlate with the objective clinical picture of the child.
Evidence for the diagnosis may include direct observation of harm, laboratory evidence (poisoning), or the abatement of symptoms with the extraction of the suspected perpetrator. Review of the literature indicates that no organ system is immune [9-12]. Consequently, it is important that the multidisciplinary team evaluate for the diagnosis of MCA and provide assistance to the child welfare and legal systems in providing documentation and testimony as well as facilitating their understanding of this complex form of child abuse [13].
Including medical child abuse in the list of differential diagnoses when the clinical picture defies logic or medical plausibility is necessary to assist in the detection of such cases. Currently the best epidemiological studies show that health professionals are likely to encounter at least one case during their careers, with pediatricians seeing many more [14]. In the last ten years, the Texas Children’s Hospital child abuse pediatric team has conducted over 100 medical investigations of suspected medical child abuse cases, with an average of 6 to 12 cases annually. As a large pediatric institution housing many notable subspecialists and clinicians, complicated and medically-challenging cases requesting further evaluation and expertise often present to the hospital.
While many of the complicated cases are indeed true and accurate, in MCA cases, the historical elements of the case do not correlate with the clinical picture of the child, and/or medical treatments provided do not produce the expected clinical effect over the course of time. There is often a slow realization by physicians that the prolonged illness may have been fabricated [7, 15]. In such cases, a cautious and conservative approach is paramount given the subtle variances and elements that must be extracted and reviewed in each case. Such case details may include:
- Doctor shopping
- Exaggeration of symptoms
- Multiple medical tests and procedures
- Subjective treatment-resistant symptoms
- Desire by the medical profession to rule out all potential medical cases
The case of the three children who experienced medical child abuse shows a number of Interest points to consider:
- The mother had brief training as a nursing student.
- A letter had been written by Charlie’s kindergarten teachers and administration citing “concern for Munchausen syndrome”, given his gaunt, thin appearance during his stays with mother, as opposed to his weeks in grandparents’ household. Additional comments included mother’s negative reactions when she was asked about the child’s prescribed medications for ADHD, and mother’s abrupt removal from the school when questioned.
- Direct communication and review of documentation of therapists and physicians revealed how mother minimized children’s progress, routinely challenged, and actually physically changed documentations of visiting therapists.
- The garage was observed to contain pallets of unopened cans of supplemental formulas which continued to be delivered, despite noting little consumption of previous deliveries.
- Mother was observed to be actively searching for medical treatments, symptoms, and various diagnoses on the internet.
- Mother’s continued quest for medical answers continued with the pursuit of a diagnosis of mitochondrial disorder, to which she herself obtained a biopsy with negative results. Medical records noted continual misrepresentation of children’s lists of diagnoses and symptoms.
- Extensive medical investigations of various conditions were duplicated by members of the same subspecialties at different institutions.
- Mother was observed to speak of children’s grave prognosis in front of the children.
- As a single mother, she was the only historian to each of the children’s symptoms.
- The exhaustive medical chart review and the creation of a timeline of events revealed an interesting and obvious pattern during each child’s hospitalizations. During these hospitalizations and periods of reported symptoms, the other children’s medical symptoms subsided. When the mother was ultimately hospitalized for an extended time, no clinical symptoms or seeking of medical attention was warranted for any child during that period or subsequently.
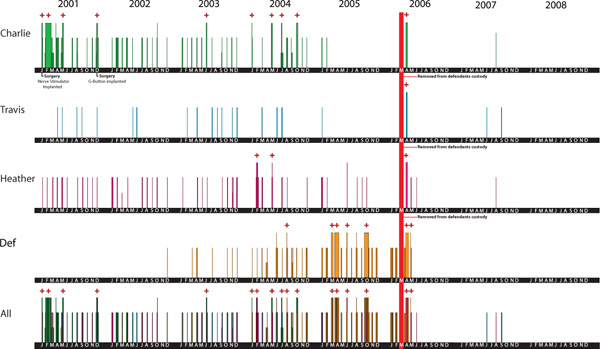
The graph represents a short window of time in the few years before and after intervention and rescue of the three children (Fig. 1). Each colored line on each patient’s axis represents a physical evaluation for that patient. The thinner lines represent a clinic or ER visit. The thicker lines represent a hospitalization. The thick red line represents the formal legal therapeutic separation of the defendant from the children, and the absolute clearing of all necessary medical visits subsequently, save for well-child visits and follow ups. A trial separation had actually begun months prior to the formal therapeutic separation, when the defendant herself was hospitalized and the children were being cared for by unsuspecting volunteers. Of further interest is the appearance of lines/visits when one child presented or was ill, and the lack of lines/visits in the others at the same point in time.
Review of the medical records and direct communication with those providing medical assessments revealed that mother displayed several techniques to facilitate symptoms and requested diagnoses:
Fabrication
The oldest child received over 22 EEGs, all but 1 EEG was considered normal, and the 1 had equivocal results. During almost all of the EEGs, the child was being prescribed multiple psychotropic medications resulting in slow EEG readings. No true seizures were objectively observed by a clinician. However, given the maternal history of persistent seizures despite optimal medical interventions, a vagal nerve stimulator (VNS) was surgically inserted to deter the reported seizures. Vomiting episodes were reported by mother for all 3 children at various points in their lives. Despite reviews of their electrolytes and other laboratory results being relatively benign and no observations of such episodes, the repeated concerning histories from the mother of vomiting and the observation of 2 of these children as thin, gaunt, and weak, gastrostomy tubes were placed in each. Starvation of the children was ultimately determined during their time of therapeutic separation from the mother.
Simulation
Observation of mother by a friend described her pressing her infant daughter to her breast during feeding and causing perioral cyanosis.
Persuasion
Mother refused to leave during children’s ophthalmologic evaluations and actively and verbally challenged children’s and clinicians observations and opinions. The mother additionally challenged occupational and physical therapists on their assessments of the children repeatedly undermining and influencing downgraded detailing of their capacities.
Induction
The mother’s intentional withholding of food and starving the children caused the children to lose considerable body weight, stunt their growth, reduce the provision of multiple medications, including psychotropics, that were ultimately realized to be unnecessary produced various symptoms and impacted the children’s quality of life. It is also suspected that she overmedicating the children causing some of their symptoms.
THE CHILD-PERPETRATOR-HEALTH SYSTEM TRIANGLE
The contract entered into by the caregiver, the healthcare professional and healthcare system is one of mutual trust and acceptance that the ultimate goal for all sides is for optimal medical care and treatment of the child patient. When one or two sides of this triangle are faulty, then the sacred contract is void. When the sacred contract of care is realized to have been broken by the inclusion of a duplicitous history or deliberate act of induction of symptoms, the physician and health care system foster feelings of betrayal and guilt in having been an unwitting player in a medical charade leading to the pain and suffering of a child.
The Child
The well-known challenge of pediatric medicine is the eliciting of a medical history from a young patient. That challenge is even greater when the patient is preverbal, or unable to offer a clear personal account of symptoms, time frames and quality of symptoms, and past medical history. The child is dependent on the caregiver for providing accurate information to the healthcare system and for providing the medically advised treatment and course. As the history still remains the cornerstone of the medical diagnosis, when the history provided is willfully deceitful, the diagnosis and treatment of the patient will inevitably be incorrect. In some cases, the patient may indeed have a true underlying medical ailment, but in cases of MCA, many of the additional flourished histories offered by an offending caregiver can cause continued medical pursuits and unnecessary testing unrelated to the true primary diagnosis.
It is not unusual for children’s voices and complaints to be overlooked. A child’s direct history is often diminished given vague reports or validated histories, despite genuine descriptions. The deflated credibility of a child alongside the elevated position of the adult caregiver enhances the opportunities for a perpetrator of MCA [16]. Older children subjected to MCA over time may come to collude with their mothers by confirming even the most fantastical tales about their medical histories [17]. The line of reality and make-believe becomes blurred for these patients, as they become accustomed to being in the sick role. The natural desire of a child to please the child’s mother or the fear of engaging the mother’s wrath if dissenting, the influence of the mother’s persuasion over time, and the likelihood that the child has come to truly believe that they are sick make the task of teasing the true medical states of these children all the more difficult [15, 18] The prognosis for child victims is dependent on the length of time the child has been forced into the sick role and the severity of the problem [15, 17] This was observed in the individual children of the presenting case study, in which the oldest sustained the abuse longer and more severely.
Characteristics of a Perpetrator
An initial review of medical child abuse in 1987 remarked that 98% of perpetrators were birth mothers of the victims [6]. Since that review, there has been a growing recognition of other perpetrators of the condition. A recent review of 451 victims of medical child abuse, found that 345 (76.5%) perpetrators were mothers, followed by the next largest group being fathers (N=30, 6.7%). In the same study, mothers were noted to have abused sons and daughters almost equally, but fathers were three times more likely to abuse their sons [7].
Perpetrators are often described in the literature as having professional training or experience in the health field, with 14.1% to 27% of perpetrators having had such training or experience in the different reviews. Many perpetrators appear very comfortable in the medical setting, are lauded by medical and nursing staff by being steadfast in their perceived perpetual care of their children and exhibiting grace under considerable pressure. In 2013, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), introduced factitious disorder imposed on another (previously factitious disorder by proxy (FDP) [19]. DSM-5 specifies identified deception by the perpetrator as an essential criterion. While the caregiver’s diagnosis or motivation is not vital to establishing child abuse, it becomes important in treatment of the caretaker’s abusive behaviors [20]. Personality disorders are not uncommon in these perpetrators.
Many caregivers will “split” medical and nursing team members, by indicating preferences for certain clinicians while “firing” others. Borderline, antisocial, narcissistic, avoidant and histrionic personality disorders are characterized in many, and high rates of these traits been identified in a systematic study of 19 mothers with fabricated illness [21]. While some may have psychiatric features associated with factitious disorder by proxy (FDP), there are external secondary gains to be made in the context of a caregiver of a sick child.
Attention-seeking is a driving motivational factor in many such cases. The need for recognition, praise, and sympathy has been recognized. A perpetrator may engage the charade of a seemingly sick child in order to redirect attention and spur a return of an absent spouse or lover. Additional external incentives in the form of financial gains and services are also lucrative. The unnatural setting of prolonged hospital life and uncertainty can also produce severe strains in the coping mechanisms of parents of chronically ill pediatric patients. Adaptive parental behaviors resulting from coping with the prolonged illness may sabotage medical care of the chronically ill pediatric patient. Such parental behaviors may be the result of unsuccessful interpersonal salvage mechanisms in the response to the strains resulting from illness in their child [22].
PHYSICIAN-HEALTH SYSTEM
Physicians enter into the health care industry primarily as a way to do social and medical good. Training in medicine includes being able elicit key elements of a patient’s medical history, perform a solid and thorough physical examination, consider the need for certain diagnostic tests, and establish a sound list of possible differential diagnoses that may contribute to the presenting medical complaint. Broad assumptions are made that all sides want the patient to be well and recover. The picture of the heroic physician who turns every stone to uncover the elusive diagnosis in a complicated, complex case may be one image of an unwitting pawn in these cases, to the perpetrator’s delight. Even for the most seasoned of physicians, the insecurity of missing something weights heavy. When challenged by peers, these physicians may become defensive and cite authority, and be reluctant to be proven wrong. Humility in a health system in acknowledging current and potential limitations mixed with hubris in being steadfast in convictions can provide an environment in which these cases can thrive. Other challenges within the health care system that can and may continue to facilitate the festering of MCA cases include [23].
The Current State of Medicine
The advent of hospitalists has reduced the need for the primary care physician to closely monitor patients during hospital admissions and to be aware of the various aspects of the medical assessments and needs. The additional inclusions of multiple subspecialists, and multiple rotating physicians within a group (whether hospitalists, primary care physicians, subspecialists) can create an environment in which medical histories are altered or misinterpreted, treatment regimen are conflicting and changing, and communications between circles are fractured. These points allow cases of MCA to flourish and/or provide cover to the perpetrator. This shift in disrupting connections between the inpatient and outpatient settings results in diminished continuity of care potentially allowing the ballooning of events and reducing the timely detection of MCA cases.
The health care industry is a business. The drive for customer satisfaction and streamlined service are commendable feats in this age of competition and comparison. However, with this comes the realization that if left unchecked continued, unnecessary medical pursuits may be conducted at the expense of the child. The lay community may not understand the limitations of diagnostic tests, and the need for prudent approaches to each medical scenario. Proceeding in a measured, sound, and judicious manner with evidence-based practices, while providing open and good communication with families, would nullify the concerns. But in today’s society with the potential negative publicity via the internet, practitioners may be reluctant to risk the wrath of the unsatisfied consumer.
Medical training that has gravitated from the bedside to the classroom has led to waning clinical experience and confidence in the history and physical examination skill sets with superficial applications [24, 25]. The technological age has introduced new diagnostic modalities that are truly remarkable affording greater visualization and detail. This and other forms of sophisticated testing in recent years have led to the predictable trend of the increased ordering of these selections [26].
Electronic Medical Record
With the hopes of improving the quality and efficiency of health care, the US Congress provided physicians and hospitals with significant financial incentives to adopt and implement the use of the electronic medical record (EMR) [27]. The EMR, while providing a streamlined system for documentation and billing for services, has been shown to be a difficult method of tracking trends and determining the beginnings of evolving cases of MCA. The summarization of cases and the cut-and-paste option for clinicians and nurses may initially seem to curtail the documentation process, but to the reviewer of cases where the details and connecting-the-dots matter, the EMR can become a vast quagmire of disjointed information. The creation of templates and pre-populated options further allow for minimal individual observations and reduce clarity of the clinical picture.
Right to Privacy
The federal Health Insurance Portability and Accountability Act of 1996 established new standards and rules that give individuals added control over how protected health information is used and disclosed. The acquisition of information between physicians and institutions has been affected given the increasing concerns of security and privacy to patient information without the written consent and cooperation of the patient and/or caregiver. While there are several sections within the Health Insurance Portability and Accountability Act that address the disclosure of information with regards to child abuse and neglect, the provision of this law can offer cloaking of cases of MCA and the effective and timely detection of cases of MCA by diminishing continuity of care.
THE INTERNET’S ROLE
The Internet has become a powerful and ubiquitous tool for those seeking information for just about every query. A report from the Pew Research Center found that 8 in 10 family caregivers (79%) have access to the Internet [28]. Of these caregivers, 88% search online for health information. These numbers underscore the vibrant quest for answers regarding signs and symptoms of a particular ailment, and understanding of diagnosis and treatment in the broad spectrum of health and medicine. The vast spider web of the net related to health issues include, but are not limited to: websites detailing certain diseases and treatment options, blogs that chronicle a patient’s medical course and personal struggles, social-networking sites that allow connections of patients and families who are afflicted with a common condition, and charity donation sites that provide a platform for solicitation of monies to meet mounting healthcare expenses. Such areas contribute to the incredible impact that the internet has had in the realm of health and science. However, along with the tremendous good that the Internet provides, comes the recognition of a new and intriguing element in investigations of medical child abuse [29].
The inclusion of the internet in cases of medical child abuse has added another dimension into the investigations of medical child abuse. The conventional wisdom has historically included the concept that a keen understanding of the health care industry with previous employment and/or training in the field was a key component in the profile of perpetrators of medical child abuse. With the advent of the internet, that line of thinking has shown to be an obsolete concept. With queries into medical scenarios and symptoms, literally at the tips of fingers, a veiled clinical picture can be constructed that mirrors true illnesses thereby stumping clinicians when diagnostic tests and examinations don’t correlate with provided medical complaints.
As attention seeking remains a significant driving force in the motivation for these types of cases, the internet can provide worldwide exposure for the perpetrators to report their experiences while garnering desired emotional secondary gains. A review of virtual journals can provide understanding and insight into motivations, while comparing the true clinical picture of a patient with a fantastical retelling online [30]. Secondary gains in the form of monetary donations and other services are also derived from the utilization of a net with a wide reach.
CONCLUSION
The legal aspect of this case of medical child abuse progressed through the civil as well as the criminal courts. The mother/perpetrator lost the parental rights of all three children. She was convicted of injury to a child and sentenced to 15 years in prison. It must be reminded that these children will bear the scars of their abuse both physically and psychologically for the rest of their lives.
Cases of child medical abuse are complex and challenging for all involved in the situation. There is some question of whether PUBLIC awareness of MCA has outpaced MEDICAL and LEGAL awareness, ironically enough. In many cases the abuse has been identified not by medical providers, but by other family members, substitute caretakers, or school personnel. Sadly, in the presenting case, school personnel raised their suspicions for MSBP six years before the children’s final intervention and diagnosis, all the while the medical community continued to believe the mother.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


