All published articles of this journal are available on ScienceDirect.
Improving Emergency Department Care to Sexual Assault Survivors Using a Risk Stratification Tool
Abstract
Background:
Sexual assault survivors who present to emergency departments are not consistently offerered prophylaxis for HIV prevention because there are currently no national evidence-based practice protocols.
Purpose:
The project aim was to improve the provision rate of (N) PEP to SA survivors by providing a decision guideline risk stratification tool and appropriate training to forensic nurses who treated SA survivors who presented within 72-hours following an assault on how to use the risk assessment and stratification tool.
Methods:
A risk stratification tool provided HIV (N) PEP clinical decision guidelines and framework for use with adult survivors. Forensic and emergency department nurses (n=20 total) were given a pre-training knowledge assessment. Forensic nurses (n = 6) were given specific training in HIV risk stratification and use of the (N) PEP decision guideline tool. Knowledge scores were assessed immediately following training and three months after implementation of the risk stratification tool.
Results:
The average knowledge score of forensic and emergency department nurses increased following training, and remained higher after three months of implementation.
Conclusion:
The implementation of a locally-specific risk stratification decision guideline tool improved both provider knowledge and patient care as measured by an increase in appropriate (N) PEP treatment rates.
Recommendations:
Further research is needed to determine if risk stratification decision tools and standardized protocols improve provider knowledge across settings such as communities with different rates of SA, HIV prevalence, and socio-economic levels.
INTRODUCTION
The Centers for Disease Control and Prevention’s (CDC) National Intimate Partner and Sexual Violence Survey for 2010 found that in the United States (U.S.) 1 in 5 women (about 31.2 million) and 1 in 71 men (about 4.4 million) have been raped in their lifetime [1]. The National Crime Victimization Survey conducted by the U.S. Department of Justice reports that every two minutes someone is sexually assaulted in the U.S. and that at least 60% of rapes/sexual assaults are not reported to the police [2]. In 2013, there were 17,844 reported incidents of sexual assault in Texas, and 129 of them occurred in Brazos County [3, 4].
In addition to physical and emotional consequences following a sexual assault, survivors face risk for pregnancy, sexually transmitted infections (STIs), including the Human Immunodeficiency Virus (HIV). There were an estimated 47,500 new cases of HIV reported in the U.S. in 2010 [5]. HIV has become entrenched across the nation, and so it has become increasingly critical for high-risk sexual assault (SA) survivors to be treated prophylactically to prevent transmission and spread of HIV. Although the risk of HIV transmission after SA is relatively low [6], but the thought of contracting the virus remains a grave and real concern to assault survivors. Characteristics of victim and perpetrator, as well as of the assault increase the risk of HIV transmission. Characteristics include: injection drug user, males who have sex with males, convicted sex offenders (HIV rates are estimated to be potentially double that of the general population), and uncircumcised males. Sexual assault survivors at greater risk of seroconverting if exposed to HIV include those who have a current sexually transmitted infection or genital lesion, have an intrauterine device, and receive a genital injury during the assault [6].
The Centers for Disease Control and Prevention recommends a post-exposure antiviral prophylaxis ([N] PEP) given up to 72 hours post-assault to reduce the risk of HIV seroconversion [7]. The CDC’s 2010 STD Treatment Guideline recommends performing a risk stratification with each SA patient that assesses: the likelihood of the assailant having HIV, any assault-specific exposure characteristics that might increase the risk for HIV transmission, the time elapsed after the event, and the potential benefits and risks associated with the (N) PEP. Because the HIV status of the assailant is often unknown, it is recommended that the provider assess all available information concerning: characteristics and HIV risk behaviors of the assailant(s), local epidemiology of HIV/AIDS prevalence, and exposure characteristics of the assault. Post SA application of (N)PEP is recommended as a routine part of care post assault for survivors presenting within 72 hours in areas with a high prevalence of HIV in the population, but not in low prevalence areas. Most health care providers are not trained in risk assessment and stratification for HIV (N) PEP in SA survivors, resulting in low rates of (N) PEP treatment in ED’s [8].
LOCAL PROBLEM
A hospital opened in Texas in 2013 which serves a rural, suburban and college community. The city is located in a rural county with a a population of 203,164 and includes two colleges which collectively have more than 75,000 students. This newly opened hospital presented a unique opportunity to train an entire staff of new forensic nurses in the use of a risk assessment tool for use with SA survivors (Table 1). Prior to the initiation of this project, this hospital did not have a standardized protocol for administering or offering HIV antiviral prophylaxis post sexual assault. Available data supports that the prevalence of HIV in Texas is of significant concern, meaning many SA survivors are potentially placed in a high risk group.
The specific aim of this project was to improve the provision rate of (N) PEP to SA survivors by providing a decision guideline risk stratification tool by training nurses who treat SA survivors on how to use the tool. This intervention project was designed to determine if the use of a clinical decision guideline/protocol to provide HIV seroconversion risk stratification would improve health care provider knowledge and attitudes, and decision making regarding the use of non-occupational post-exposure prophylaxis in SA patients who presented within 72 hours post-assault. This project focused strictly on providing information regarding decisions related to the provision of (N) PEP, but not on adherence or follow up of the patients with the (N) PEP medications.
METHODS
Ethical Issues
Approval for this quality improvement project was obtained through the Committee of Human Subjects at The University of Texas Health Science Center. All forensic and emergency room nurses in the emergency department (n= 20) who volunteered to participate were assigned a randomized participant code by the Interim Assistant Chief Nursing Officer, and their identities were withheld. Tests with ID codes only were retained by the investigator separate from the hospital to assure data integrity and anonymity of participants. Retrospective chart reviews were performed three months after the implementation of training program after all identification from charts were removed to ensure patient privacy. Data from SA cases were presented only in aggregated form to ensure patient confidentiality. No conflicts of interest were identified in the present study.
| Risk Category | Clinical/Historical Findings | Recommendation for Non-Occupational Post Exposure Prophylaxsis | Medication Recommendation |
|---|---|---|---|
| High |
• Penetration assault by one or more assailants known to be HIV positive or at high risk of HIV infection. (Injection drug users, men who have sex with men)* And/or • Anal penetration with or without injuries.** |
Strongly Recommended | Truvada, (Emtracitabine, 200 mg/Tenofovir 300mg), 1 tablet po daily X 28 days Kaletra (Lopinavir 200 mg/ Ritonavir 50 mg), 2 tablets po twice daily X 28 days |
| Moderate High |
• Penetration assault by one or more assailants of unknown HIV status with vaginal injuries and known or unsure ejaculation and no or uncertain condom use. • Penetration assault in the presence of sexually transmitted infection, genital lesion, IUD, menstruation. • Penetration assault by one of more uncircumcised assailants of unknown HIV status. |
Recommended | As per High Risk |
| Moderate Low | • Penetration assault by one or more assailants of unknown HIV status with no vaginal injuries-with ejaculation or vaginal injuries without ejaculation | Optional | As per High and Moderate High Risk |
| Low |
• No anal or vaginal penetration • No ejaculation from the assailant • Oral penetration only • Condom use • Assailant known to be HIV negative • Bite injury unless the biters mouth was bloody and the exposed patient’s skin is visibly broken |
Not Recommended | None |
Setting
The participating hospital sought to improve care provided to SA patients in accordance with best evidence-based medicine practices given the consequences of HIV exposure, especially in light of the large population of college students served. The Forensic Nursing team was all female, Caucasian, and between the ages of 29 and 45, with two advanced practitioners, two were bachelor’s degree prepared nurses and two were associate degree nurses.
In 2013, over 4000 new cases of HIV were reported in Texas (DSHS, 2014). In 2013 in the Texas county where the hospital is located, 322 people were living with HIV and an additional 25 new cases were reported [9]. This relatively high local incidence of 158 HIV cases/100,000 population, coupled with the increase of 7% of HIV cases in a single year indicates that concern among SA survivors about HIV exposure risks is warranted.
Intervention Plans
This project was designed to examine the impact of the implementation of an HIV risk stratification decision guideline tool and training to Forensic Nurses in a Central TX Emergency Department on provider knowledge of proper HIV risk stratification and on proper (N) PEP treatment to SA survivors. A risk stratification tool was adapted with permission from the University of Pittsburgh Medical Center – Hamot’s Forensic program. Using CDC guidelines the tool was updated based upon local experiences and demographics, including the estimated HIV prevalence within the county, and to ensure clarity, accuracy and ease of use. The revised risk stratification tool (Fig. 1) was provided as a paper version that Forensic Nurses could access and utilize easily during the course of post-SA examinations.
Prior to tool distribution, the Forensic Nurses (n = 6), along with other ER nurses (n = 14) at the hospital were given a pre-training assessment to determine a baseline of existing levels of knowledge of HIV risk stratification at their monthly in service training session (Table 2). Following completion of the pre-training assessment the forensic department nurses (n=6) were trained via a session that utilized PowerPoint and oral presentations, as well as written materials about HIV risk stratification and the proper use of the risk stratification tool and N (PEP) protocols. During the training presentation, simulated case examples were used to increase nurses comfort and awareness of the procedures involved in risk stratification. Immediately following this one hour training session, a post-training assessment was given to the forensic department nurses (n=6) to determine the effectiveness of the training session. The difference in knowledge scores between pre and post- training was defined as immediate knowledge impact.
| Pre-Intervention | Post-Intervention | 3 months post Intervention | |
|---|---|---|---|
| Mean knowledge scores + Standard error | 6.3+0.494a | 11.1+0.6 b | 8.3+0.71 a, b |
Three months after implementation of the risk stratification tool, an additional HIV risk stratification knowledge assessment was given to all the Forensic Nurses (n=6). The score on this test demonstrated long-term knowledge retention and assimilation (long-term impact) (Table 2). Comments and attitudes about the risk stratification tool were also collected at this time using an anonymous Qualtrics survey that assessed opinions using a Likert scale (1=most useful, 5 = not useful).
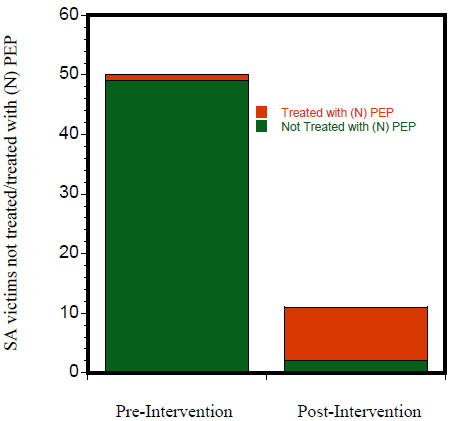
Methods of Evaluation
A retrospective SA case chart review over a 12 month period was performed three months following the implementation of the (N) PEP protocol. The case review was divided into two periods: the nine month period prior to training and implementation (pre-intervention), and for the three months after training (post-intervention). Each SA case (n=50 pre-intervention cases and n = 11 post intervention cases) during these two periods was blinded for personally identifiable information, and was assessed for appropriate HIV risk stratification and (N) PEP treatment. Proper risk stratification of each SA case was confirmed both by the principal investigator and an independent secondary non-affiliated chart reviewer doctorally prepared sexual assault advanced practice nurse familiar with HIV risk stratification post-SA. All SA cases were identified by inclusion in SA reports from the participating hospital and were evaluated for potential inclusion in the present study based on patient age (>18 years of age) and length of time after assault (< 72 h) and their treatment was evaluated according to the present risk stratification guidelines. The difference in correct (N) PEP provision rates was determined to be the impact of the nurse training and risk assessment tool use on patient care. The raw percentage of appropriately (N) PEP treated patients were compared between the two pre and post-intervention periods. There was no attrition of nursing participants during the study period. Although the study size was relatively small (n = 20), the sample included the entire population of Forensic Nurses in this hospital, ensuring local validity and applicability and by including the larger set of total nurses, we were able to establish a true baseline of knowledge of staff who encounter SA survivors on a routine basis. Knowledge scores over time relative to the training were compared to determine: 1) immediate training effectiveness, and 2) long-term knowledge retention. Proper (N)PEP provision to SA survivors was the ultimate metric for determining effectiveness of the training on provider knowledge and skills and patient care.
Following the three month implementation period, an informal online survey tool was used to gauge the ease of use and effectiveness of the risk stratification from participating nurses. Questions included asking the nurses to evaluate the usefulness, applicability, ease and provider attitudes toward HIV (N) PEP and how these were impacted by the training and use of the HIV risk stratification tool in helping to determine a patient’s risk of acquiring HIV. In general, the responses were all positive and indicated that the risk stratification tool increased provider comfort and confidence in providing specific information about HIV risks and prophylaxis to SA survivors.
Analysis
Repeated measure analysis of variance (ANOVA) was conducted to compare the knowledge scores of the forensic nurses before and after risk stratification training as well as after three months of implementation. The knowledge assessment instrument underwent content validation by 10 nursing experts with a resulting content validity ratio of 0.88 [10]. The stepped-up consistency version for determining intra-class correlation coefficients (ICC) was conducted across the 10 raters for the assessment. The total mean scores across five separate ratings from each evaluator was ICC = 0.91 indicating very high inter-rater reliability.
RESULTS
Post hoc comparisons revealed a significant increase in mean knowledge scores for the participating nurses (n=6) on the post training assessment from baseline (m=6.33, SD=1.21) compared to immediately following the intervention (m-11.83, SD=1.47, p=0.001). Mean knowledge scores after three months of implementation collection period were significantly lower than the post intervention scores (p=0.036). No significant differences were observed between baseline (pre intervention) and three months post intervention, but the mean knowledge scores were numerically higher (Table 2).
In the nine months prior to the training intervention, according to a chart review, only one SA patient out of 50 had been identified and offered N (PEP), a 2% compliance rate (Fig. 1). Eleven (11) charts met inclusion criteria during the three month implementation period and 81% of the patients were correctly risk stratified. The use of the risk assesment tool was overall rated highly by the participating nurses with a mean score of of 4.2, SD = 0.84 out of a 5 point scale (n=5). In the informal survey, nurses reported a better understanding of risk stratification regarding HIV post exposure (M= 3.2 and SD of 1.30, n=5) the results were neutral to agreement that they had a better understanding (data not shown). There was a single outlier value at 1, and removing this outlier resulted in a M=3.75 with the majority feeling they had a better understanding of HIV risk factors and the need for HIV (N) PEP in SA victims.
DISCUSSION
While the exact risk of HIV transmission in patients post sexual assault is unknown, the risks of transmission in consensual sexual acts are known. If a person participates in receptive anal intercourse, there are 50 transmissions/10,000 acts; receptive penile-vaginal intercourse 10 transmissions/10,000 acts; insertive anal intercourse 6.5 transmissions/10,000 acts; and both receptive and insertive oral intercourse are very low risk [6]. However, transmission probabilities are greater in acute and late phases of HIV infection when both plasma and genital HIV viral concentrations are higher. Furthermore, the minimal infective dose of HIV remains unknown in humans. Most importantly, from the point of view of a SA survivor, submucosal replication of HIV occurs within hours of exposure. Collectively, these facts underscore the need for immediate HIV prophylactic action in the wake of a sexual assault, while the course of action must be based upon evidence-based risk factors specific to each SA and the local HIV prevalence rates.
The lack of a national guideline for HIV prophylaxyis has caused difficulties for care providers of SA survivors because they lack specific information on evaluating the risks of HIV transmission to an individual survivor. Therefore risk stratification tools have been devised at several locations around the country to reduce the burden of judgement on care providers by providing specific protocols along with a risk stratification tool for use with SA survivors. The present project showed the introduction of a risk stratification tool improved the identification of at-risk SA survivors and their need for HIV (N)PEP.
In a chart review of female sexual assault patients (>18 years of age) in the emergency department of Boston Medical Center, several factors were associated with offering HIV (N) PEP [11]. In this study, 229 charts were reviewed and the final sample size enrolled was 181 SA survivors, and HIV (N) PEP was offered to 89 (49%) of patients [11]. Using multivariate analysis there were three variables associated with the decision to offer (N) PEP: 1) stranger assault, 2) any type of patient insurance, and 3) being under 33 years of age [11]. The guidelines that were in place at the time of the study were the 2002 CDC guidelines which acknowledged a risk from assault, but did not recommend (N) PEP [12]. An Australian study found that out of 146 post sexual assault survivors who presented to a Sydney Emergency Department, (N) PEP would have been appropriate treatment for 117 victims, but only 9 (7.7%) of which received a prescription [13]. Other authors found that the chance of receiving a prescription for (N) PEP varied depending on the type of assault with those who were anally assaulted being the most likely to receive or be offered treatment [14, 15]. When prescribed (infrequently), (N) PEP was prescribed in accordance with the then-current guidelines [13]. The researchers pointed out the difficulty of collecting accurate, comprehensive information in the acute phase following a sexual assault, and acknowledged a potential for bias [13]. Collectively, the evidentiary literature recommendations for practice include: 1) developing a clinical decision tool that rapidly, efficiently, and accurately assesses the risk of HIV transmission following sexual assault, 2) developing evidence-based, standardized HIV (N) PEP protocols tailored to meet community needs, and 3) consultation with multi-disciplinary experts to provide education and training on use of (N)PEP guidelines/protocols/tool. Additional studies indicated that since the publication of updated guidelines in 2010 HIV (N) PEP has been offered more frequently [16, 17]; however, the rates remain remarkably low. Studies that provided site-specific guidelines and /or protocols were most successful at offering HIV (N) PEP appropriately [16].
Limitations
Limitations to the present study include the use of a small sample size of both participating nurses and the number of SA case charts reviewed. Because the nurses were new to forensic nursing (<6 months experience) with limited practical experience, the results may not reflect those of more experienced providers. Generalizability of the study is somewhat limited based on population size and general demographics of the area. However, the findings suggest that training in, and use of a risk stratification tool improved nurses knowledge of HIV transmission and risks associated with SA and patient care as measured by appropriate HIV (N) PEP treatment was increased.
Interpretation
Similar to the Templeton et al. [13], study, the initial offering of (N) PEP at the present hospital was low (7.7% versus the present 2%). Following the training and implementation of a post SA risk stratification decision tool the rate of (N) PEP compliance increased to over 80%. Nurses that had been trained in the use of this tool felt more comfortable in assessing the need for (N) PEP in SA patients and their knowledge scores increased significantly following training. While the gain in testable knowledge appeared to dissipate after the three month implementation period, the improvement in patient treatment results and the comfort of nurses use of a risk stratification tool remained.
CONCLUSION
A new hospital was challenged by multiple victims of sexual assault presenting to the Emergency Department in the absence of a patient care protocol, specially educated staff, or a tool to assist in making decisions about HIV (N) PEP prophylaxis. During planning and implementation of this project, the Forensic Nursing department was formed and began to function within the hospital, simultaneously a Sexual Assault treatment protocol was created and staff were educated and trained in use of a risk stratification decision making tool. Furthermore, by educating staff appropriately about the risks of HIV transmission, patients were more well-informed of their personal risks following a sexual assault. Collectively, the present results, as well as the literature demonstrate an increase in provider knowledge and willingness to provide HIV (N) PEP when provided with appropriate training and tools, resulting ultimately in a reduction in HIV infections following high risk sexual assaults.
Implications from this study indicated that increasing provider education and giving them appropriate tools and guidelines improved provider confidence and education levels and ultimately improved patient care relative to (N) PEP treatment. Results of the present study support a more detailed investigation of the impact of HIV risk stratification tools for the provision of (N) PEP post sexual assault. Future studies should include a multisite wide-scale implementation of a locally-specific HIV risk stratification training and tool in a step-wise process. An extentsion of this study would utilize the same tool modified for local needs and conditions at multiple hospitals and measure the impact of training and the use of a risk assessment tool on improved patient care for an extended period of time to improve reliability and generalizability.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


