All published articles of this journal are available on ScienceDirect.
Urinary Retention Secondary to Colpocleisis: A Case Report
Abstract
Introduction:
Pelvic Organ Prolapse (POP) is common in older women, and depending on its extent, it is conservative or surgically treated. Colpocleisis is a technique for POP treatment, in which the vaginal canal is closed, entirely or partially, in order to avoid the protrusion of the pelvic structures, with preservation of the urethral meatus in order to preserve normal micturition.
Clinical Case:
We present a case of a 61-year old woman, who 8 years after a colpocleisis, progressed to urinary retention associated with the progressive scarring of the labia, causing the obstruction of the urethral meatus. The patient underwent a labiaplasty with anterior colpoperineoplasty, with complete normalization of her micturition and sexual activity.
Conclusion:
Long term urinary retention complication has not been previously reported in the literature and should be included as a possible adverse event after colpocleisis.
1. INTRODUCTION
Pelvic Organ Prolapse (POP) is the protrusion of the pelvic organs through the introitus vaginalis, caused by the rupture or dysfunction of the endopelvic fixation structures, accompanied by the weakening of adjacent tissues [1]. POP can affect the quality of life of those who suffer from it because it can cause lower abdominal, sacral or lumbar pain, sexual dysfunction, dyspareunia, urinary incontinence, increased post-void residual urine, constipation, vaginal bleeding, hematuria or hemato- chezia [2].
The women's health initiative study describes that 41% of postmenopausal women without hysterectomy and 38% of hysterectomized postmenopausal women presented some degree of POP [3] as a result of inadequate vaginal vault suspension.
POP is classified into 4 grades: grade I, the pelvic organs protrude beyond the lower half of the vagina without reaching the hymen; grade II, the prolapsed organs reach the hymen; grade III, the vaginal dome exits beyond the hymen, although the vagina is not fully everted; while grade IV involves the complete vaginal eversion [4]. Another classification is to consider a complete POP when there is any degree of hysterocele (with or without cysto or rectocele) and an incomplete POP when only one of the vaginal walls (anterior or posterior) is involved [5].
Incomplete POP or grades I and II are routinely observed or managed conservatively with rehabilitation exercises of the pelvic floor muscles [6], hormone replacement or pessaries, in contrast to complete POP or grades III and IV, in which surgical treatment is the treatment of choice; the surgical treatment is classified into 3 groups: reconstructive surgery that reinforces the endogenous support of the pelvic structures; compensatory surgery, which replaces the deficient support with a synthetic (mesh) or allogeneic (autologous fascia, cadaveric or bovine) graft; and finally, obliterative surgery in which the POP is treated by partial or total occlusion of the vagina which includes colpectomy or colpocleisis [7], depending on the removal, or not, of the vaginal tissue.
Colpocleisis is a simple technique for POP treatment, in which the vaginal canal is closed, entirely or partially, in order to avoid the protrusion of the pelvic structures, with preservation of the urethral meatus in order to preserve normal micturition [8, 9]. This procedure is a quick and simple procedure that improves the patient’s quality of life and restores bladder and bowel function. Colpocleisis is only indicated in elderly women with complete POP and does not involve functional repair due to co-morbidities, and in women who do not want to preserve their sexual function because it involves the occlusion of the vagina [9]; the priority of this procedure is to achieve a quick, simple, low complication approach with efficiency and durability with the POP repair [1].
There are two types of colpocleisis: total colpocleisis, in which the vaginal space is fully occluded through binding integumentary and mucosal tissue, from the hymen ring posterior up to 0.5-2.0 cm of the external anterior urethral meatus; and a partial colpocleisis, in which the distal portion of the vagina wall is preserved with the closure of the labia [1].
Most women with symptomatic POP are treated with reconstructive procedures [9], with a low risk of recurrence. Colpocleisis is another option with low morbidity and adequate efficiency because it is a less invasive surgery and a good choice for women who do not desire vaginal intercourse. Another limitation after colpocleisis is the inability to evaluate the cervix and uterus vaginally, limiting the diagnosis of certain gynecologic illnesses [8].
2. CLINICAL CASE
A 61-year-old Mexican a healthy woman, arrived at the urologist's office describing difficulty during micturition, which reaches the point where it is practically impossible. The medical history included a vaginal hysterectomy 8 years earlier with oophorectomy and a colpocleisis for POP. The colpo- cleisis was performed without the patient’s knowledge, consent or discussion of the surgical sequelae. When questioned during the medical interview, she mentioned that after the surgery, she was unable to have vaginal intercourse and developed stress urinary incontinence without adequate voiding, which has increased progressively. She was treated for 7 years by a gynecologist with an estrogen cream. During the last year, she had experienced increasing voiding difficulty, reaching a point in which she could only partially void “by flexing on her belly without urine exiting out of the body, but feeling certain relief and that something was filled”, and when she stood up, her urine leaked into the diaper.
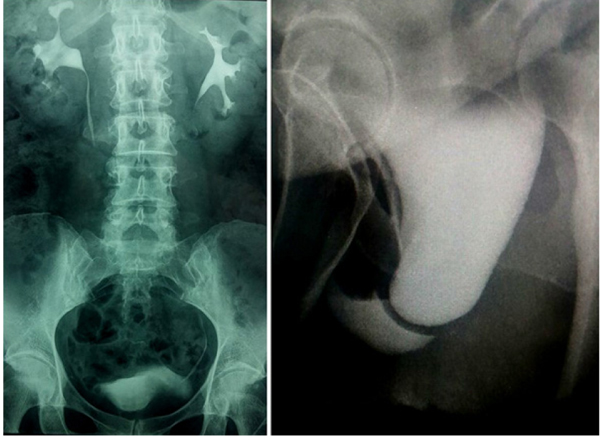
The physical examination demonstrated a full bladder that was palpable with complete closure of the introitus; the patient had a total fusion of the labia that did not allow the urethral meatus to be visible (Fig. 1).

An intravenous excretory pyelography was performed because it was impossible to place a Foley catheter for a retrograde cystography because the urethral meatus was impossible to locate or visualize. A progressive bladder prolapse was associated with the extrinsic compression of the abdomen, without any urine leakage, and during the voiding phase, the vagina was filled with urine, associated with an incomplete bladder emptying and vaginal collection of the voided urine (Fig. 2).
The patient underwent a labiaplasty with resection of the anterior vaginal mucosa as part of the anterior colpope- rineoplasty, obtaining an excellent cosmetic result. She was discharged 18 hours later with a Foley catheter for 72 hours with adequate spontaneous micturition, without incontinence and an adequate opening of the vagina (Fig. 3). In her follow-up visits 1 and 3 months after the surgery, she had normal bladder voiding without incontinence, with an adequate open vaginal introitus and normal vaginal intercourse (Fig. 3). On her physical exam, her genitalia looked normal, with scarcely good scar tissue, normal vaginal exam, without urine leak coughing nor with Valsalva maneuver.

3. RESULTS AND DISCUSSION
Colpocleisis is routinely recognized as a minimally invasive technique with high success rate (above 90%), short surgery time (between 58 to 156 minutes) [10], low complication rate (6.82%), and very low mortality rate (0.4 to 0.15%) [11, 12]; it is recommended for elderly women with POP. The complications most frequently reported include bladder injuries during dissection, urinary urgency or stress incontinence due to the change in the trigone position, increased postvoid residual volume, recurrence of the POP because of further prolapse as well as wound, uterus or urinary tract infection [13, 14]. Moreover, complications associated with a surgical procedure include local infection, urinary tract infection, bleeding, myocardial infarcts and sepsis [15].
The first complication in this woman was the violation of her rights, as she was not provided with sufficiently clear, timely and accurate information of what a colpocleisis procedure involves, in order to freely choose her treatment (it is important to emphasize that she was a healthy 53-year-old woman with incomplete POP as her only complaint before the initial surgery). The colpocleisis procedure performed led her to lose her vaginal sexual activity without adequate knowledge of consequences, because as we have mentioned before, she had not been explained the type of procedure she was undergoing and its significance. After the colpocleisis surgery, the patient developed urinary incontinence, probably associated with the urodynamic changes induced because of the distortion of the anatomy of the pelvic organs [16]; this adverse effect of colpocleisis is well reported in the literature.
There was progressive scarring at the labial surgical site, which closed the meatus, causing urinary retention. This late complication (8 years later) was due to the mechanical obstruction of the urethral meatus by the progressive fusion of the labia, causing bladder emptying dysfunction. The diagnosis was clinical based on the impossibility to visualize or place a Foley catheter for the cystography to confirm the clinical diagnosis, which was further confirmed with the contrast study.
The surgical repair included labiaplasty and anterior colpoperineoplasty without synthetic mesh placement because of the quality of the vaginal tissues under the continuous estrogenic stimulation. The preference of avoiding the use of a prosthetic mesh was based on current indications that only after an informed consent of the patient regarding the risk of mesh erosion (10%), wound granulation (8%), dyspareunia (9%) and infection [17], could it be placed. And given the excellent quality of the tissues and the medical history of our patient, this type of reconstruction was preferred.
CONCLUSION
Female candidates to undergo a colpocleisis must be thoroughly informed of the procedure and the complications before the surgery is performed, including secondary urinary retention that can be an infrequent and late complication in women undergoing colpocleisis and which should be evaluated during their follow-up.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The bioethics committee of the Hospital Angeles de Puebla reviewed these letters and agreed that all personal information of the patient was secure and that international protocols were followed (Approval No. 2019-19E/cirugía.).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 1983.
CONSENT FOR PUBLICATION
The patient has signed an informed consent as well as a letter regarding protection of her privacy.
STANDARDS OF REPORTING
CARE guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


