All published articles of this journal are available on ScienceDirect.
Back to Basics: The Identification of Genital Anatomic Structures and Forensic Evidence Collection Kits in Cases of Suspected Child Sexual Abuse
Abstract
Background:
The genitalia examination and collection of forensic evidence are essential components of the medical evaluation when sexual abuse is suspected. In addition to a complete history/interview, the medical visit for a suspected child sexual abuse victim usually includes a detailed examination of external genitalia and anus as well as, if indicated, the collection of forensic evidence. It is important that medical and nursing professionals are able to correctly identify normal genital and anal structures before they can identify abnormal physical findings in either the prepubertal or adolescent patient. Additionally, medical and nursing professionals are expected to accurately collect and preserve forensic evidence when possible.
Methods:
A topical review of literature that examines: 1) if physicians and nurse practitioners could identify basic anatomic structure of external genitalia, and 2) the timing and yield of forensic evidence collection kits.
Results:
Physicians vary in their ability to correctly identify prepubertal genital anatomic structures. Over a series of studies, on the same photograph of female prepubertal genitalia, 59 to 64% of physicians correctly identified the hymen from; 76 to 90% correctly identified the labia minora, and 63 to 78%correctly identified the urethra. On a second photo, deemed more clear, 71% of pediatric chief residents correctly labeled the hymen. Pediatric nurse practitioners performed similarly to the physicians correctly identifying the hymen 59%, labia minora 88% and urethra 81%. Looking at photographs of male prepubertal genitalia, 93% of pediatric chief residents correctly identified the basic structures while only 22% correctly recognized hypospadias. Literature reviewed on forensic evidence collection kits support an extended window for evidence collection of up to 96 hours after suspected sexual contact especially of clothing and other non-body surfaces.
Conclusion:
Medical and advanced practice nursing professions have to improve the educational processes of clinicians who evaluate and treat children suspected of abuse. Physicians and nurse practitioners experienced difficulty in correctly labeling and identifying basic external genital structures on a photograph of a prepubertal child’s genitalia. Additionally, extending the time frame from suspected sexual contact to examination to a window of up to 96-hours post assault may increase the yield of recovering forensic evidence in both pre and post-pubertal patients.
INTRODUCTION
The medical and nursing professions seek to improve the training and education of professionals who evaluate children suspected of child abuse and neglect [1-6]. As the theory base and clinical skills needed to identify and treat child abuse and neglect have proliferated over the past four decades, educational approaches to help clinicians become more proficient in the evaluation and treatment of maltreatment have also expanded [7]. In 2009, the field of child abuse pediatrics came to the foreground in medical education with the emergence of a board certified subspecialty in child abuse with a more focused approach to general and specialty training for physicians who evaluate and care for child abuse victims [8, 9].. Literature supports the recommendation that child maltreatment curricula ought to comprehensively address how clinicians can best assess children suspected of child abuse, better identify cases of abuse, and then intervene to treat and protect a child [10]. Studies have shown that clinicians are not consistent in correctly identifying genital anatomic structures that are important to know when evaluating a child suspected of sexual abuse [5, 7, 11, 12]. This article reviews the research that highlights the skills necessary to identify the anatomic structures of the external genitalia in children and to assess the timing and yield of forensic evidence collection.
The current 21st century knowledge base of child abuse and neglect content has grown exponentially since the landmark publication of the “battered child” by Kempe and colleagues in 1962 and Kempe’s recognition of sexual abuse as a “hidden problem” in 1978 [13, 14]. There has been an improvement in ability of clinicians caring for children suspected of abuse to determine plausible diagnoses of abuse and neglect, and then have those findings hold up in a court of law. Such improvement is due to an emphasis on specialized education focusing on the details and nuances of all aspects of child maltreatment. It is imperative for clinicians to have specific training in child abuse in order for them to correctly evaluate the child and identify abuse, and then make appropriate referrals to other professionals such as child protective services (CPS) and law enforcement investigators who help protect the child physically and legally. It takes a solid knowledge base to complete a history and physical examination to evaluate for the possibility of abuse as well as conditions that might mimic abuse. The child maltreatment literature highlights differences in the knowledge base and competency of clinicians who have further training in abuse and those who do not [6, 9, 11, 15].
The educational preparation of a clinician who evaluates a child suspected of child abuse or neglect does affect the ability to determine the presence or absence of abuse findings. Knowledge of anatomy is the beginning point of competency in child sexual abuse evaluation [16]. Studies conducted over the past 30 years have shown that clinicians want more training and education in child abuse and neglect, and feel more confident in diagnosis and treatment options when they have had more specialized training in the identification, assessment and treatment of a child suspected of abuse [12, 17-20]. The competent child abuse clinician knows how to conduct a complete evaluation that includes a medical history, physical examination, collection of forensic evidence, and determining appropriate laboratory and imaging studies. Clinicians also need to recognize non-abuse related medical conditions that mimic findings suggestive of sexual abuse.
The genitalia examination is an essential component of the medical evaluation when sexual abuse is suspected. The medical visit for a suspected child sexual abuse victim usually includes a detailed examination of external genitalia as well as evaluation of the anus. As such, it is reasonable to expect that if a clinician is unable to correctly identify normal genital and anal structures in the prepubertal or adolescent patient, then the identification of abnormal findings may not be possible either. Evidence in the peer reviewed literature confirms that the majority of child sexual abuse cases will not have any abnormal genital findings present on the child’s genital examination [21-23]. So, it is essential for the examining health care professional, either a physician or nurse practitioner, to be skilled at identifying both normal and abnormal genital anatomy so as to correctly evaluate the suspicion of abuse and then to be able to explain any findings, or the lack of findings, during the examination.
PHYSICAL EXAMINATION OF GENITALIA IN SUSPECTED CHILD SEXUAL ABUSE
The clinical approach to a comprehensive evaluation of a child suspected of sexual abuse involves first obtaining a thorough medical history, and then conducting a head to toe physical examination, including the genital area. Studies have shown that introducing a child to the components of the exam and the colposcopic equipment prior to experiencing the exam helps to decrease the child’s anxiety and distress related to the ano-genital exam [24-26]. Factors that seem to contribute to more adverse responses from the child during an exam include caregiver anxiety and response to outcry, significant cognitive disability in the patient, a history of more invasive forms of sexual abuse, a chronic medical diagnosis, an ano-genital exam requiring anal or genital cultures, and uninsured status [24, 25].
A thorough healthcare evaluation of suspected child sexual abuse includes [27]:
- A detailed history of present illness – from the child as well as caregiver statements – in addition to an appropriate medical history
- A complete head to toe physical examination
- Appropriate laboratory tests, diagnostic testing and imaging studies
- The collection of evidence - including photo-documentation and physical (forensic) evidence collection
- Knowledge of the differential diagnoses that mimic child abuse and neglect
- A clinical impression and working diagnosis
- Meticulous documentation of all medical information
The collection of forensic evidence is a learned skill and as such is best done by trained professionals, be they child sexual assault nurse examiners (SANEs), child abuse pediatricians, or emergency room physicians with experience in forensic evidence collection [28, 29]. Sievers [30] compared the accuracy of use of evidence collection kits collected by SANE nurses to those collected physicians and nurses who were not SANE trained. The study found that evidence collected by SANEs was more likely to have appropriately labeled and sealed specimen envelopes, a completed chain of custody, appropriate amounts of swabs, head and pubic hair, collected blood, and vaginal motility specimens than those collected by non-SANE-trained nurses and physicians. The results may suggest that further training in any skill or process produces more accurate outcomes than when a clinician is not trained in specific areas of practice.
The anogenital exam is a necessary component of a child’s medical evaluation when there is suspicion of inappropriate contact. In such cases, the forensic evidence kit (FEK) is used to collect evidence during the course of the exam [28, 29].
FEK contents may vary by county and state. All should include an instruction sheet and documentation forms, as well as paper bags and envelopes for holding evidence. Swabs are needed for collecting vulvar, vaginal, and anal samples as well as cervical samples in a subset of patients. A comb for pubic hair collection and an orange stick for hyponychial samples are also helpful.
During the exam, the clinician collects hair and other body secretion samples, and documents physical findings using photography where appropriate. The child’s clothing, including underwear, is bagged appropriately, along with blood and urine samples.
All samples are collected, carefully packaged to avoid contamination, and stored in refrigeration. Chain of custody is maintained at all times until an investigative officer transports the kit for analysis. Ideally, the medical facility should provide fresh clothing and undergarments at the time the child is discharged.
Physicians and advanced practice nurses are typically the clinicians who complete the comprehensive medical evaluation of a child suspected of sexual abuse [1, 2, 31]. Although corroborative findings, such as forensic evidence, anogenital injury, or sexually transmitted infections may be found in some patients, the medical diagnosis of child sexual abuse derives primarily from a clear history of abuse or assault provided by the pediatric patient.
Legal and child welfare agencies use medical information to make crucial decisions that further affect the safety of the child, and any other minors in the same environment. The details collected in the medical evaluation guide the overall investigation conducted by child protective services (CPS) and law enforcement agencies [32]. The examining clinicians must collect medical facts and also document findings in a way that renders the pertinent history and examination data understandable throughout the course of the investigation by non-medical personnel and into the courtroom setting.
LITERATURE REVIEW
The following is a topical review of studies that determined how well physicians and nurse practitioners identify basic anatomic structures of the external genitalia when provided with photographs taken during a genital examination. A series of 4 studies using photographs of pre-pubertal female genital anatomy and 1 study that examined male prepubertal anatomy are summarized. Additionally, several articles that address the optimal timing and yield of the FEK are also reviewed and summarized.
RECOGNITION OF BASIC GENITAL ANATOMY
Female Prepubertal Examination
A series of survey studies conducted over a ten-year period used a photograph of female prepubertal genitalia to determine if physicians and nurse practitioners could identify basic anatomic structures of the external genitalia. Four separate studies to determine clinicians' ability to identify external genitalia structures of prepubertal females found that a significant proportion of the respondents were not able to correctly label the hymen [33-35].These studies found that physicians and nurse practitioners experienced difficulty in correctly labeling and identifying basic female external genital structures on a photograph of a prepubertal child’s genitalia [33, 34] (See Fig. 1).

In the first of the photograph identification studies series, Ladson Johnson, and Doty [33] analyzed questionnaires received from 129 physicians, including family practitioners, pediatricians, and pediatric residents. When given a photograph of the external genitalia of a prepubertal female child, only 59.1% of physician respondents were able to correctly label the hymen (See Table 1).
| Ladson et al. (1987) (n=129)‡ |
Lentsch and Johnson (2000) (n=166)† |
Dubow et al. (2005) (n=139)* |
Hornor, McCleery (2000)^ | |
|---|---|---|---|---|
| Respondents | Family practitioners, pediatricians, and pediatric residents | General and specialty trained pediatricians, family practitioners, and emergency medicine specialists | Pediatric chief residents | Pediatric nurse practitioners |
| Photo used | Fig. (1a) | Fig. (1a) | Fig. (1a) | Fig. (1a) |
| Anatomy Structures | Correctly Identified (%) | Correctly Identified (%) | Correctly Identified (%) | Correctly Identified (%) |
| Clitoris | 89 | 94 | 94 | 91 |
| Posterior commissure | 81 | 87 | 87 | |
| Urethra | 78 | 72 | 63 | 81 |
| Labia minora | 76 | 83 | 90 | 88 |
| Labia majora | 62 | 79 | 80 | |
| Hymen | 59 | 62 | 64** | 59 |
A decade later, Lentsch and Johnson [34] conducted a second study similar to the Ladson, et al., methodology where they surveyed 166 general and specialty trained pediatricians, family practitioners, and emergency medicine specialists. They found that physicians did not routinely check the prepubertal genitalia. The survey also found that although physicians did consider sexual abuse as a cause of sexually transmitted infections (STI), they were less likely to report their suspicions as possible sexual abuse depending on the STI [34]. When asked to identify anatomical structures on a photograph of a female child’s prepubertal genitalia, only 61.7% of physicians labeled the hymen correctly. The study concluded that physicians did not consistently recognize normal female prepubertal genital anatomy, and that physician ability to identify prepubertal genital structures correctly had not improved since the Ladson, et al. [33], study 10 years prior (See Table 1).
The third identification series study examined the recognition skills of pediatric nurse practitioners. Hornor and McCleery [35] analyzed 83 responses from pediatric nurse practitioners to the same photograph of the female child’s prepubertal genitalia [35]. The study findings showed that 58.8% of pediatric nurse practitioners respondents identified the child’s hymen on the photograph. This finding was similar to the two physician groups of prior studies (See Table 1).
The fourth study surveyed 139 pediatric chief residents to identify anatomic structures on the same photograph from the previous surveys [36]. Dubow, Giardino, Christian and Johnson found that only 64% of respondents correctly labeled the hymen. The pediatric chief residents performed similarly to the other physician and nurse practitioner groups. An assumption that pediatric chief residents might be better trained than pediatric residency graduates because of the selection process for chief residents did not translate into better performance on structure identification [36] (See Fig. 1 and Table 1).
The results of the chief resident study showed that the pediatric chief resident respondents were better able to identify a number of anatomic structures compared to the physicians in the 1986 Ladson, et al. [33], study (59.1%) and were on par with the Lentsch and Johnson [34] study (61.7%). The Dubow, et al. [36], chief resident study concluded that the physician responses still showed deficiencies in clinician ability to recognize genitalia structures in the normal prepubertal female. Additionally, the authors suggested that residency programs need to improve training efforts to improve physician ability to identify anatomical structures of the genitalia and in turn improve the accuracy of the genital examination in prepubertal children.
Muram, et al. [37], investigated the effect of an educational intervention on the ability of clinicians to first recognize features and structures of the prepubertal female genitalia and to diagnose common gynecologic conditions. Overall, the group of 20 faculty members, 40 residents and 2 nurses as a whole correctly identified approximately half the cases of normal and abnormal exams. Attending physicians performed slightly better than residents, but the difference was relatively small. Neither were there significant differences between residents at the various levels of training. In accord with the Ladson, et al., and Lentsch and Johnson [33, 34] studies decades earlier, many participants had difficulties identifying normal features of a female genital exam with less than half of the respondents correctly identifying either normal features of the prepubertal anatomy or anatomic variants of normal. Surprisingly, many participants had a tendency to label examinations, both normal and abnormal, as indicative of sexual abuse of the female patient in question.
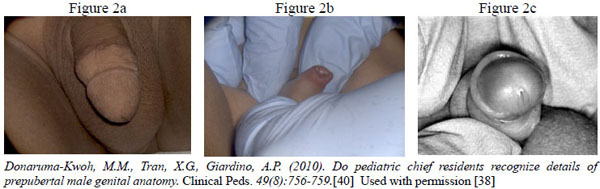
Male Prepubertal Anatomy
Donaruma-Kwoh, Tran, and Giardino in 2010 [38] studied the ability of pediatric chief residents to identify pre-pubertal male genital anatomy. Nearly 93% of respondents were able to identify the basic structures on a picture of a circumcised male, while only 22% correctly recognized hypospadias as an example of an abnormal finding in the same gender and age group [38] (See Fig. 2 and Table 2). The Donaruma-Kwoh, et al., survey also focused on practice procedures in evaluating male genital anatomy, formal education regarding the male anatomy, and experience with medical testimony in sexual abuse cases [38]. In comparing the clinical practice of female versus male chief residents, female chief residents were more likely than their male counterparts to include a genital exam in a routine physical examination for infants and prepubertal boys. In response to identifying normal male anatomy in photographs, 96% of chief resident respondents correctly identified male genital anatomy, 96% identified an uncircumcised penis, while only 22% correctly identified an abnormal condition. When respondents were asked about their level of confidence to serve as a medical expert, 2% felt confident in their ability, 94% did not feel confident, and 4% were uncertain. Chief resident performance in this study, identifying male genital anatomic structures, was superior when compared to the performance in the study measuring correct identification of normal female genital anatomy. Given the inability of chief resident respondents to correctly identify hypospadias as an abnormal finding, the researchers recommended that pediatric residency training should address the male genitalia exam in greater detail [39].
| Anatomy Structure | Results (%) (n=108)ª |
|---|---|
| Structure of male anatomy (urethral meatus, glans, and penile shaft) | 92 |
| Circumcised penis | 96 |
| Uncircumcised penis | 96 |
| Tanner stage | 84 |
| Abnormal Condition (hypospadias) | 22 |
Related Considerations
Documentation of Genital Examination Findings
Makoroff, Brauley, Myers, Brandner, and Shapiro [5] studied the documentation of genital examination findings to compare the accuracy of findings by physicians with training in child sexual abuse to findings of physicians with no additional training in child abuse. Pediatric emergency medicine (PEM) physicians with training in child abuse reviewed abuse specific diagnoses made by pediatric emergency physicians with no additional training in child abuse. The chart review found that physicians with no training in child sexual abuse were not accurate in correctly diagnosing abuse in children, and in fact, over-diagnosed normal exams as indicative of sexual abuse. The child abuse trained physicians found that in the children who were evaluated by physicians with no additional training in child abuse, only 17% of the children suspected of sexual abuse truly had abnormal findings consistent with sexual abuse. The study recommended that emergency medical physicians have additional training in abuse, and that children diagnosed with abnormal findings should be reevaluated by clinicians who have training in child abuse.
Forensic Evidence Collection Kits
Timing
The most useful time frame for the collection of evidence from the child’s body is still a question under investigation. The sophistication and sensitivity of DNA analysis techniques has increased in the last two decades and many current studies encourage a conservative approach of 72 hours to completing the FEK with a time window similar to that of adult women.
A landmark study in the field of timing for collection of evidence after a reported assault in sexual abuse is a retrospective review of forensic tests of 273 children less than 10 years of age [40]. Christian, et al., noted that 25% of the children had positive forensic evidence extracted from samples collected at emergency department visits. Sixty-four percent of the positive findings were found on clothing or bedding, whereas only one child seen after 24 hours had bodily evidence (a foreign pubic hair) preserved [40]. These findings led to the recommendation that when an evidence kit is collected, clothing and linens should be pursued vigorously for analysis, while evidence collection from the child’s body surface was not likely to be necessary after 24 hours [40].
A 2006 retrospective review of consecutive pediatric patients seen within 72 hours of their assault found that providers at a community child advocacy center described certain case characteristics that were predictive of evidence detection. Overall, 9% of the study population had positive forensic evidence isolated. Semen or sperm was identified from body swabs only from non-bathed, female children older than 10 years of age or on clothing or objects [41]. Similar results were discovered in another retrospective review in a hospital setting. Of the forensic findings of children and adolescents who had FEK completion within 72 hours of an abusive event, 81% of the positive findings were from patients older than 12 years old and the remaining 19% of pre-pubertal patients had evidence recovered from clothing and linens [42]. These results were consistent with the findings from the 2000 study by Christian, et al. [40].
Ten years after the Christian, et al. study [40], a retrospective review of all pediatric patients (aged 0-20 years) who underwent FEK collection showed that 25% of their cases had FEKs with forensic findings. Identifiable DNA was collected from a child’s body despite several perceived barriers: (1) cases in which evidence collection was performed greater than 24 hours beyond the assault; (2) the child had a normal/non-acute anogenital examination; (3) there was no reported history of ejaculation; and, (4) the victim had bathed and/or changed clothes before evidence collection [43]. The authors concluded that failure to conduct evidence collection on pre-pubertal children beyond 24 hours after the assault will result in missed opportunities to identify forensic evidence, though these will be rare cases [43].
Finally, a study was conducted that determined the relationship between time of sexual assault and the time frame in which the yield of evidence using DNA amplification is valid supported an extended time frame for FEK collection from children [44]. Findings showed that body swabs collected from children beyond 24 hours after assault still yielded evidence. The majority of children with isolated perpetrator DNA from their bodily samples were aged 10 or older, but kits from 14 children younger than 10 also had a positive DNA results: 5 were positive by a body swab collected between 7 and 95 hours after assault. Body swabs were important in the collection of evidence for older children, but body swabs were significantly less likely than non-body specimens to yield DNA from pre-pubertal children [44]. Authors concluded that despite a limited yield of positive findings, clinicians should consider the collection of body samples from children beyond 24 hours after assault. They further concluded that findings on physical examination do not predict what forensic laboratory tests might show [44].
Additional Considerations to the Physical Exam
A recent survey of pediatric chief residents at each of the 187 pediatric residency programs in the United States which had a 64% response rate found that nearly 90% of the programs included training in child maltreatment, but only 25% of the programs had an actual child abuse and neglect curriculum in place [45]. There was a statistically significant association between the number of sessions of child maltreatment training and resident confidence in recognizing child abuse and neglect, taking a maltreatment history and knowledge of ethnic and cultural practice. Residents in programs with a written curriculum expressed more perceived confidence across these three areas as well. Pediatricians in practice after their residency training also report a sense of discomfort with child maltreatment exams, particularly those where the chief complaint is sexual abuse [46]. In this survey of AAP members, the majority of respondents had little experience evaluating and reporting suspected child abuse or neglect, and reported interest in having expert consultation. Pediatricians in this sample felt competent in conducting medical exams for suspected maltreatment, but felt less competent in rendering a definitive opinion, and did not generally feel competent to testify in court. Increased practice experience and more education on abuse topics led to increased sense of competence in some areas.
While familiarity with the genitalia is an obvious component of the competent clinical assessment, the medical literature reflects a lack of comfort and a scanty knowledge base for practitioners who are called to deal with this patient population.
CONCLUSION
A clinician’s ability to diagnose a case of child maltreatment is an essential first step in the efforts to keep children safe and healthy. There may be severe consequences for the child, family, and community when a healthcare practitioner misses the signs and symptoms of an abused or neglected child. An inaccurate or inadequate medical evaluation of a child suspected of abuse may result in returning that child to an unsafe environment. Conversely, an overzealous diagnosis of child maltreatment can have devastating consequences for all involved. The misdiagnosis of abuse when it is not present may cause children and families to undergo unnecessary investigations and be separated from their caregivers; additionally, a misdiagnosed case of abuse may allow medical conditions to go untreated if other diagnostic possibilities are not carefully considered [18, 47]. A correctly diagnosed case of abuse allows for an appropriate response to keep the child safe.
A medical evaluation approached in a knowledgeable and sensitive manner may be a first step in the child’s healing, especially when the healthcare provider communicates care, respect, and interest in the safety of the child and their family [1-4, 48, 49]. Clearly, the physical examination skills of the clinician are an important aspect of the training. The literature summarized in this paper suggests that the medical and advanced practice nursing professions have to improve the educational processes of clinicians who evaluate and treat children suspected of sexual abuse victimization.
The studies discussed in this paper suggest the need for physicians and nurses to improve their knowledge of basic genital anatomy. A clinician’s ability to first identify genital structures and then to know what comprises normal and abnormal findings is an essential first step in the evaluation of a child suspected of having been sexually abused. Additionally, the recommendations to aggressively pursue collection of undergarments and other available non-body sources for detection of perpetrator DNA are important, and should be followed by all practitioners. Extending the time frame for forensic evidence collection out to the 96 hour period has advantages for pediatric patients particularly around undergarments and available non-body sources.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


