All published articles of this journal are available on ScienceDirect.
Rate of Vascular Access Preparation in Hemodialysis Patients and Associated Baseline Characteristics in Jazan Region, Saudi Arabia: A Multicentre Study
Abstract
Background
End-stage renal disease (ESRD) treated with hemodialysis is a major global health concern. Delayed preparation for renal replacement therapy can lead to adverse consequences. We aimed to determine the rate of vascular access preparation in hemodialysis patients and the associated baseline characteristics in the Jazan region, Saudi Arabia.
Methods
This is a cross-sectional observational study using patients’ medical records and complimentary direct patient interviews during their hemodialysis sessions in different Jazan region centers.
Results
The study included 310 patients, of which 58.1% were male, 45.5% aged 40 to 60 years, and 50% were non-Saudi. Hypertension was the cause of end-stage renal disease (ESRD) in 42.6% of participants, with renal artery stenosis and lupus being the least common causes. Regarding the association between ESRD causes and demographic factors, we found only age and marital status were statistically significant. We also found that only the education level is statistically associated with early referral for vascular access placement.
Conclusion
ESRD was more common among middle-aged males, and hypertension was the most likely cause. Our study showed that the arteriovenous fistula was used only in 50% of patients as vascular access for hemodialysis. Compared to other demographic factors, education level has significantly affected the early referral rates for vascular access placement.
1. INTRODUCTION
Chronic kidney disease (CKD) is rapidly being recognized as a significant health threat that is associated with premature mortality and substantial social and economic consequences. It is considered an independent risk factor for various health issues including cardiovascular diseases, cognitive dysfunction, increased rate of hospitalization, and all-cause mortality [1, 2].
In the Kingdom of Saudi Arabia (KSA), chronic kidney disease (CKD) is a critical health concern. Currently, there are approximately 20,000 patients undergoing renal dialysis in Saudi Arabia. The cumulative prevalence of both modalities of renal replacement treatment in Saudi Arabia is predicted to be about 300 per million population [3].
There is a universal agreement that patients with CKD should undergo multidisciplinary clinical preparation for at least six months before starting renal replacement therapy (RRT) [4]. Adequate preparation before RRT is essential to maximize the patient's quality of health status [5]. The CKD patients who are adequately prepared for RRT in the form of regular screening and monitoring have exhibited a slower decline in kidney function, shorter hospital stay, and reduced rate of death before reaching the end stage. The screening and monitoring programs include early referral to a nephrologist, education, management of comorbidities and complications, early placement of dialysis access, adequate time initiation of dialysis, and pre-emptive kidney transplantation [6-8].
According to the KDIGO Guideline (Kidney Disease Initiative Global Outcomes), the patients should be prepared when they reach stage four (estimated glomerular filtration rate 15-30 ml/min/1.732) [9]. However, it has been shown that CKD patients are far more likely to die than to attain RRT because it was instituted lately [10-12].
In the United States, over 110,000 patients with end-stage renal disease (ESRD) begin their maintenance hemodialysis every year. However, there’s a significant proportion of CKD patients who are inadequately prepared for RRT even those who are referred earlier to the nephrologists. Moreover, the vast majority of patients who are already on hemodialysis lack permanent vascular access [13].
In a large retrospective study conducted on 1057 French patients who started dialysis between 1989 and 1998, the 5-year cardiovascular survival was found to be significantly lower in patients who had been referred late (less than 6 months) compared to those who had been referred earlier (between 3 and 6 years) or more than 6 years (57.8% vs 77.1% vs 65.3%), respectively before the start of hemodialysis [14].
To the best of our knowledge, there is a lack of data regarding the preparation rate for hemodialysis in Saudi Arabia, reflecting this study’s importance. This study is the first to be conducted in the region to address this issue. It aims to determine the rate of vascular access preparation in hemodialysis patients and their baseline characteristics.
2. MATERIAL AND METHODS
2.1. Study Setting, Design, and Population
This cross-sectional observational study used patients’ medical records and direct patient interviews during their hemodialysis sessions. Using a prespecified data collection template, the data had been collected from patients' files and recorded. Any missing data in patients’ charts had been gathered from the patients directly during their HD sessions. We conducted our study in different hemodialysis centers in Jazan. Jazan region is located in the southwest of Saudi Arabia, with a population of 1.6 million people based on the last census report. There are eight dialysis centers affiliated with MOH that serve around 1,153 hemodialysis patients throughout the region [15].
Our study targeted all adult patients (> 18 years) with ESRD who are already on hemodialysis and performing their hemodialysis sessions essentially in Jazan. Those who declined consent to participate in the study, pediatric patients, and those who have ESRD as a result of acute kidney injury (AKI) were excluded from this study.
2.2. Sample Size and Sampling Technique
The study followed the simple random method of sampling. The Raosoft sample size calculator (http://www. Raosoft.com/samplesize.html) was used for sample size estimation. Given that the population size of dialysis patients in the Jazan region is about 1153 hemodialysis patients with a 95% confidence interval and leaving 5% for sample error; thereby, the estimated minimum sample size was 310 individuals. We divided this number propor- tionately among the eight dialysis units to get a representative sample for all dialysis patients.
2.3. Study Instruments and Data Collection Method
After consenting the eligible patients, the data were gathered by the study investigators who were distributed over the different HD centers. The variables of data collection included demographic and clinical character- istics (age, gender, education level, monthly income, marital status, nationality, residence, and the cause of ESRD) and hemodialysis data (prior screening for CKD, whether patients had referral early for hemodialysis or not, reasons for late referral, current vascular access). The preparation is considered late if patients with advanced CKD have urgent indications to initiate hemodialysis without previous attempts for arteriovenous vascular access placement or if preparation started when eGFR has fallen below 5-7 ml/min/1.732 [16].
2.4. Statistical Analysis
All data were entered into Microsoft Excel 2016. We used Microsoft SPSS (Statistical Product and Service Solutions, version 27, 2020) for statistical tests. We presented our descriptive statistics in numbers and percentages. We used the Chi-square test to find out the relations between the data variables. A two-sided p-value of <0.05 has been considered an indicator of statistical significance. Tables and figures have been used to express the results.
2.5. Ethical Approval
The study was reviewed and approved by the Research Ethics Committee-MOH in Jazan. Approval No.:22060; date:29 June 2022. For participants whose data were not available in the electronic system, informed consent was taken. The research participants were assured that there was no harm from this study. Respect for the dignity of the research participants was prioritized. The anonymity of individuals participating in the research was guaranteed. Data collected from study participants were used only for scientific purposes. All participants had the right to stay or withdraw at any time from the study. Any misinformation and representation of the raw data results in a biased manner were avoided. All data obtained from participants through hospital records were kept in a safe place with high confidentiality.
3. RESULTS
In this study, we were able to collect data from 310 patients in the Jazan region during the period from August 2022 until June 2023. Among the participants, 58.1% were males. The age of 45.5% of the participants was between 40-60 years, while 27.4% of them were between 20-40 years. Only one-fifth of this cohort aged more than 60 years (21.3%). Saudis and non-Saudis were distributed equally in this study. In terms of marital status, 72.9% of the participants were married while 23.5% were single. More than half of the study participants were illiterate (57%) while only 6.8% had attained a university level. Considering monthly income, we found that most of the participants (81.3%) reported having a monthly income of less than 4000 Saudi Arabian Riyal (SAR) while 2.9% of them reported earning a monthly income of more than 8000 SAR (One U$ = SAR 3.75). Moreover, we found that around two-thirds of the participants were living in rural areas (62.6%) (Tables 1-2).
| Criteria | Number | Percent |
|---|---|---|
| Gender | ||
| Female | 130 | 41.9 |
| Male | 180 | 58.1 |
| Age | ||
| <20 | 14 | 4.5 |
| 20-40 | 85 | 27.4 |
| 40-60 | 141 | 45.5 |
| 60-80 | 66 | 21.3 |
| >80 | 4 | 1.3 |
| Nationality | ||
| Saudi | 153 | 49.4 |
| Non-Saudi | 157 | 50.6 |
| Marital Status | ||
| Divorced | 3 | 1.0 |
| Married | 226 | 72.9 |
| Single | 73 | 23.5 |
| Widow | 8 | 2.6 |
| Level of Education | ||
| Illiterate | 176 | 56.8 |
| Primary school | 58 | 18.7 |
| Secondary school | 55 | 17.7 |
| University | 21 | 6.8 |
| Monthly Income | ||
| <4000 | 252 | 81.3 |
| 4000-7999 | 49 | 15.8 |
| 8000 + | 9 | 2.9 |
| Residence | ||
| Rural | 194 | 62.6 |
| Urban | 116 | 37.4 |
| Reasons for Late Referral | Number | % |
|---|---|---|
| No data | 196 | 77.7 |
| No CKD screening by primary physicians | 31 | 12.3 |
| Referred but the system delayed the process | 15 | 7.0 |
| Referred but the patient refused the referral | 10 | 4.0 |
| Total | 252 | 100 |
Hypertension (HTN) was implicated in 42.6% of patients as a cause of ESRD, followed by diabetes mellitus (DM) in 16%. The reasons for ESRD in eighteen percent of patients were unknown. Cardiac diseases, inherited diseases, chronic glomerulonephritis (CGN), Renal artery stenosis, and systemic lupus erythematosus (SLE) represented the minority of ESRD causes among our study participants (<10% each) as demonstrated in Fig. (1).
Our study sought to identify the reasons for the late referral of patients with chronic kidney disease (CKD) to nephrology specialists. In 77.7% of cases, we did not reveal any clear reason for late referral. This would be due to a lack of documentation or information on the patient's CKD status or referral history. The second most common reason was the absence of CKD screening by physicians, which accounted for 12.3% of cases. Referred but “the system delayed the process” accounted for 7.0% of cases. “Referred but the patient refused” accounted for 4.0% of all cases.
As shown in Fig. (2), most of the ESRD patients are referred late to the Nephrology specialists (81%).
In terms of current vascular access, we found that only half of the participants have an arteriovenous fistula (AVF) as a current vascular access, while internal jugular Perm cath represented 40% of hemodialysis accesses. Moreover, a femoral Perm catheter was used in 4.8% of the participants. Arteriovenous grafts (AVG) and inferior vena cava dialysis catheters have been reported in 2.3 and 2.9%, respectively as shown in Table 3.
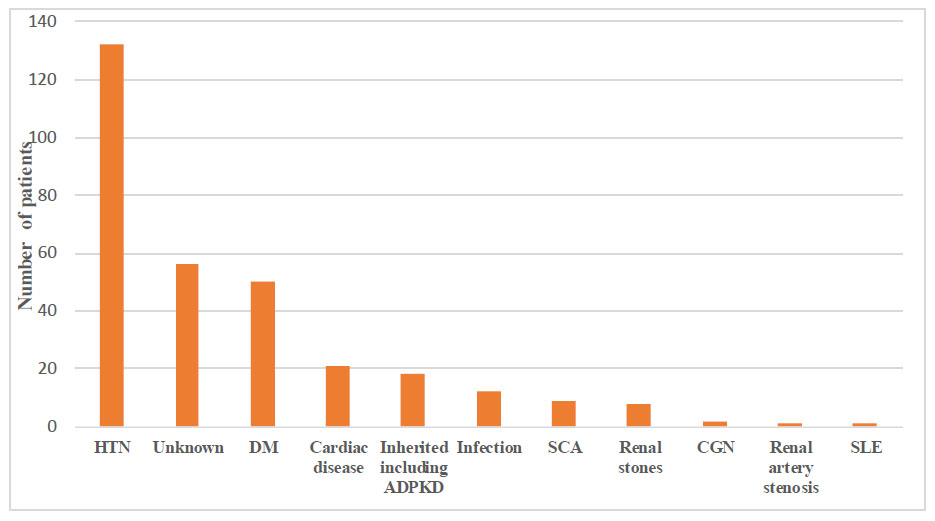
Causes of ESRD in Jazan.
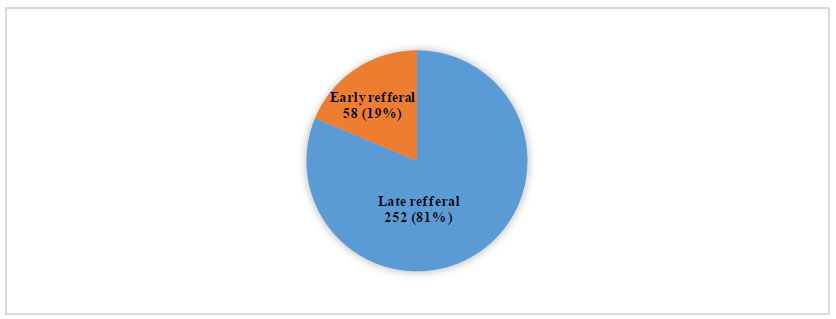
Early versus late referral of ESRD patients for hemodialysis preparation.
In terms of the association of ESRD causes with demographic variables, we found that the patients aged between 40-60 years were reported to be more likely to have HTN, DM, and unknown etiology as causes of their ESRD compared to their counterparts (P <0.001). Obviously, younger patients (<40 years) are more likely to have inherited diseases. ESRD secondary to diabetes mellitus, hypertension, or unknown etiology is more common among married individuals. No statistically significant differences were found in the other variable categories in association with the causes of ESRD as shown in Table 4.
With regard to whether early referral for hemodialysis was related to the patients’ demographic variables, we found that the illiterates were the least patients who were referred early for RRT compared to the patients who attained primary, secondary, or university levels of schools (13% vs 27.6%, 25.5%,23.8%, respectively). No statistically significant association was found with regard to other variables and early referral for dialysis preparation Table 5.
| Vascular Access | Number | Percent |
|---|---|---|
| AVF | 155 | 50.0 |
| IJ Perm cath | 124 | 40.0 |
| Femoral Perm cath | 15 | 4.8 |
| IVC | 9 | 2.9 |
| AVG | 7 | 2.3 |
| Total | 310 | 100.0 |
| Variables | DM | HTN | Infection | Inherited | Others | Unknown | Total | P |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male | 28 (15.6%) | 66 (36.7%) | 8 (4.4%) | 11 (6.1%) | 30 (16.7%) | 37 (20.6%) | 180 (100%) | >0.05 |
| Female | 22 (16.9%) | 66 (50.8%) | 4 (3.1%) | 7 (5.4%) | 12 (9.2%) | 19 (14.6%) | 130 (100%) | |
| Age | ||||||||
| <20 | 0 (0.0%) | 1 (7.1%) | 1 (7.1%) | 4 (28.6%) | 2 (14.3%) | 6 (42.9%) | 14 (100%) | <0.001 |
| 20-40 | 9 (10.6%) | 30 (35.3%) | 5 (5.9%) | 10 (11.8%) | 16 (18.8%) | 15 (17.6%) | 85 (100%) | |
| 40-60 | 25 (17.7%) | 72 (51.1%) | 5 (3.5%) | 3 (2.1%) | 16 (11.3%) | 20 (14.2%) | 141 (100%) | |
| 60+ | 16 (22.9%) | 29(41.4%) | 1 (1.4%) | 1 (1.4%) | 8 (11.4%) | 15 (21.4%) | 70 (100%) | |
| Residency | ||||||||
| Rural | 32 (16.5%) | 80 (41.2%) | 9 (4.6%) | 8 (4.1%) | 30 (15.5%) | 35 (18.0%) | 194 (100%) | >0.05 |
| Urban | 18 (15.5%) | 52 (44.8%) | 3 (2.6%) | 10 (8.6%) | 12 (10.3%) | 21 (18.1%) | 116 (100%) | |
| Marital Status | ||||||||
| Single | 10 (23.7%) | 20 (27.4%) | 5 (6.8%) | 12 (16.4%) | 11 (15.1%) | 15 (20.5%) | 73 (100%) | 0.01 |
| Married | 36 (15.9%) | 107 (47.3%) | 7 (3.1%) | 6 (2.7%) | 31 (13.7%) | 39 (17.3%) | 226 (100%) | |
| Divorced | 1 (33.3%) | 1 (33.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (33.3%) | 3 (100%) | |
| Widow | 3 (37.5%) | 4 (50.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (12.5%) | 8 (100%) | |
| Educational Level | ||||||||
| Illiterate | 33 (18.8%) | 81 (46.0%) | 5 (2.8%) | 7 (4.0%) | 18 (10.2%) | 32 (18.2%) | 176 (100%) | >0.05 |
| Primary School | 9 (15.5%) | 22 (37.9%) | 6 (10.3%) | 6 (10.3%) | 6 (10.3%) | 9 (15.5%) | 58 (100%) | |
| Secondary School | 8 (14.5%) | 20 (36.4%) | 1 (1.8%) | 3 (5.5%) | 14 (25.5%) | 9 (16.4%) | 55 (100%) | |
| University and above | 0 (0.0%) | 9 (42.9%) | 0 (0.0%) | 2 (9.5%) | 4 (19.0%) | 6 (28.6%) | 21 (100%) | |
| Nationality | ||||||||
| Non-Saudi | 17 (10.8%) | 72 (45.9%) | 7 (4.5%) | 12 (7.6%) | 20 (12.7%) | 29 (18.5%) | 157 (100%) | >0.05 |
| Saudi | 33 (21.6%) | 60 (39.2%) | 5 (3.3%) | 6 (3.9%) | 22 (14.4%) | 27 (17.6%) | 153 (100%) | |
| Monthly Income (In Saudi Riyals) | ||||||||
| <4000 | 44 | 108 | 10 | 16 | 29 | 45 | 252 | >0.05 |
| 4000-8000 | 5 (10.2%) | 23 (46.9%) | 2 (4.1%) | 0 (0.0%) | 12 (24.5%) | 7 (14.3%) | 49 (100%) | |
| 8000+ | 1 (11.1%) | 1 (11.1%) | 0 (0.0%) | 2 (22.2%) | 1 (11.1%) | 4 (44.4%) | 9 (100%) | |
Table 5.
| Variables | Late Referral | Early Referral | Total | P |
|---|---|---|---|---|
| Gender | ||||
| Male | 142 (78.9%) | 38 (21.1%) | 180 (100%) | >0.05 |
| Female | 110 (84.6%) | 20 (15.4%) | 130 (100%) | |
| Age | ||||
| <20 | 9 (64.3%) | 5 (35.7%) | 14 (100%) | >0.05 |
| 20-40 | 72 (84.7%) | 13 (15.3%) | 85 (100%) | |
| 40-60 | 113 (80.1%) | 28 (19.9%) | 141 (100%) | |
| 60+ | 58 (82.9%) | 12 (17.1%) | 70 (100%) | |
| Residence | ||||
| Rural | 153 (78.9%) | 41 (21.1%) | 194 (100%) | >0.05 |
| Urban | 99 (85.3%) | 17 (14.7%) | 116 (100%) | |
| Marital Status | ||||
| Single | 63 (86.3%) | 10 (13.7%) | 73 (100%) | >0.05 |
| Married | 178 (78.8%) | 48 (21.2%) | 226 (100%) | |
| Divorced | 3 (100%) | 0 (0.0%) | 3 (100%) | |
| Widow | 8 (100%) | 0 (0.0%) | 8 (100%) | |
| Educational Level | ||||
| Illiterate | 153 (86.9%) | 23 (13.1%) | 176 (100%) | 0.03 |
| Primary School | 42 (72.4%) | 16 (27.6%) | 58 (100%) | |
| Secondary School | 41 (74.5%) | 14 (25.5%) | 55 (100%) | |
| University and above | 16 (76.2%) | 5 (23.8%) | 21 (100%) | |
| Nationality | ||||
| Non-Saudi | 133 (84.7%) | 24 (15.3%) | 157 (100%) | >0.05 |
| Saudi | 119 (77.8%) | 34 (22.2%) | 153 (100%) | |
| Monthly Income | ||||
| <4000 | 208 (82.5%) | 44 (17.5%) | 252 (100%) | >0.05 |
| 4000-8000 | 36 (73.5%) | 13 (26.5%) | 49 (100%) | |
| 8000+ | 8 (88.9%) | 1 (11.1%) | 9 (100%) | |
| Cause of ESRD | ||||
| DM | 44 (80.0%) | 6 (12.0%) | 50 (100%) | >0.05 |
| HTN | 107 (81.1%) | 25 (18.9%) | 132 (100%) | |
| Infection | 7 (58.3%) | 5 (41.7%) | 12 (100%) | |
| Inherited | 15 (83.3%) | 3 (16.7%) | 18 (100%) | |
| Others | 35 (83.3%) | 7 (16.7%) | 42 (100%) | |
| Unknown | 44 (78.6%) | 12 (21.4%) | 56 (100%) | |
4. DISCUSSION
This study involved 310 hemodialysis patients; the majority were middle-aged males at 40-60 years. This observation is in line with both the local and global data, which indicate that a peak incidence of ESRD in such age groups is likely due to conditions such as hypertension and diabetes causing renal damage over time [3, 17-20]. The equal distribution of Saudis and non-Saudis possibly reflects the large expatriate workers population in Saudi Arabia [21]. Over half of the group was illiterate, and only 6.8% had attained a university education, which could contribute to the lack of awareness about kidney disease risks and complications [22, 23]. Individuals with lower levels of education have been found to have an increased risk of ESRD, complications of hemodialysis, and mortality [22]. A notable proportion of the group had low income, which can create financial barriers to accessing healthcare services [24]. Most patients in this study are residing in rural areas, where access to health care services is typically more limited in the region [3, 19, 24].
In the current study, we found that the most prevalent cause of ESRD was hypertension. Two studies conducted in Brazil showed the same finding (15–16). However, DM was the most common cause of ESRD, as reported in other two studies in Brazil and Palestine (17–18). This illustrates the disastrous consequences of these two silent killers and necessitates increased efforts to improve awareness among such populations to promote the prevention of their complications. On the other hand, cardiac disease, inherited diseases, infections, sickle cell disease, and renal stones are important but far less frequent causes. Moreover, 18% of our patients had an unknown cause of their ESRD. This could be due to the lack of optimal kidney health care services provided in the region as most patients are not referred to higher centers to perform renal biopsies or because of the nationality and financial status of the studied patients. However, most CKD patients have several risk factors that include diabetes, high blood pressure, heart disease, obesity, a family history of CKD, inherited kidney disorders, and older age [20, 23]. As such, it is crucial to educate individuals, especially those with a low education level, about the risk factors and complications of CKD to prevent the progression of kidney disease and its associated health problems and to inform the stakeholders to improve the medical services in this discipline.
Most patients in our study (81%) were referred late to nephrology care. Late referral increases morbidity and mortality in patients with advanced CKD [25-29]. There is a wide variation in the literature on the frequency of referral of advanced CKD patients for placement of vascular access. In a study held in northern India for instance, they found that the percentage of people with CKD referred late to nephrologists has reached up to 52% [30]. Several studies conducted worldwide on this matter showed heterogeneity in early referral rate for vascular access placement with most of them indicating a low early referral rate emphasizing that an ongoing challenge worldwide [31-36].
In our study, we found that the second most common reason for late referral was the absence of CKD screening by physicians, which accounted for 12.3% of cases, followed by the system delaying process which accounted for 7.0%, then it followed by patient refusal which accounted for 4.0% of all cases. The reasons for late referral, such as lack of screening and patient refusal, highlight the need for greater awareness and better communication around CKD risks and complications in the Saudi population [37]. Strategies like automatic eGFR reporting and education for primary care physicians could help improve screening and early referral [38]. It is also essential to empower patients through health literacy efforts to understand their disease better and to educate them about the importance of nephrology care [39]. A survey conducted on nephrologists in the Kingdom of Saudi Arabia revealed several factors contributing to the delay in AVF creation, including patient denial of kidney disease or the need for AVF (76.4%), fears and practical concerns about hemodialysis (75.9%), and patient refusal (73.1%) [40].
A well-functioning vascular access (VA) is essential for carrying out an effective hemodialysis (HD) procedure. The native arteriovenous fistula (AVF) is the best VA option due to lower rates of complications such as infectious, thrombotic risks, hospitalizations, and mortality compared to arteriovenous grafts (AVG) and central venous catheters (CVCs). Although AVG and CVCs would be alternative options in certain conditions [41, 42]. Despite the fact that the KDOQI guidelines recommend using AVFs as the preferred vascular access for hemodialysis patients whenever possible, our study showed that only half of the patients were using them. However, the guidelines may not be feasible to achieve the 50% target AVFs as primary vascular access at the facility level because the creation and maintenance of an AVF can be challenging [42]. The rate of AVFs in our study was lower than the rates in other countries such as Germany (84%), France (77%), Italy (90%), the United Kingdom (67%), Egypt (67.3%), Palestine (69.3%), Al-Khobar, Saudi Arabia (56%) as well as Riyadh in Saudi Arabia [43-47]. However, it was higher than the proportion of AVF utilization in Ireland (45%). In our study, we found that the second most commonly used VA was CVCs (45%), including both internal jugular permcath and femoral permcath, which was much higher than other countries such as France (6%), Germany (4%), Spain (7%), the USA (15%), and Palestine [10, 46-52]. Collectively, our region has a lower prevalence of AVF and a higher proportion of catheters than developed nations. Given the favorable outcomes associated with AVFs placement, the regional decision-makers should be strict on the guidelines and make the necessary arrangements to ensure optimal renal care delivery to our hemodialysis patients.
Regarding the association between the causes of end-stage renal disease (ESRD) and demographic variables, in our study, we found that older patients were reported to be more likely to have HTN, DM, and unknown etiology as causes of their ESRD. A study conducted in India in 2014 found that there is a significant association between ESRD and advanced age [53]. Another study conducted in Korea found a direct association between age and the development of CKD as well as an increased incidence of the elderly having additional risk factors of CKD [54]. Moreover, a study conducted in China in 2022 found that aged participants are more susceptible to hypertensive nephropathy than younger participants [55].
Age is a significant risk factor for the development of ESRD, and the relationship between age and the causes of ESRD is complex. Inherited kidney diseases, such as polycystic kidney disease, are more common among younger individuals and can lead to ESRD. These conditions are typically genetic and can cause the kidneys to gradually lose their function over time. On the other hand, chronic diseases such as diabetes, hypertension, and cardiovascular disease are more common among middle-aged and older individuals. These conditions can cause damage to the kidneys leading to chronic kidney disease and eventually ESRD [56-58].
It is worth noting that while these age ranges are expected for the development of certain conditions, ESRD can develop at any age and can have various causes. Other risk factors such as obesity, smoking, and a family history of kidney disease can also contribute to the development of ESRD regardless of age. Overall, understanding the relationship between age and the causes of ESRD can help inform strategies for prevention and early intervention to reduce the risk of developing this condition [58, 59].
In the current study, we found that there is no relationship between the educational level and the cause of ESRD. This finding is consistent with a case-control study conducted in Sa’ada City, Yemen, which found that the educational level had no relation to ESRD cause [60]. However, another study conducted in the Netherlands found that there is a significant association between educational level and elevated risk of causes of ESRD, increased incidence of diabetes, and other modifiable risk factors including abdominal obesity, smoking, low potassium intake, and hypertension, showing that those who are less educated are thought to be more likely to have this association [61].
Our study also showed that there is a statistically significant association between marital status and the causes of ESRD. The finding is similar to another study conducted in Cameroon where a significant relationship to the causes of ESRD existed [62]. Nevertheless, it is known that family and social status independently affect the well-being of ESRD patients [63]. The association of marital status with the development of ESRD could be explained by several factors. For example, married individuals may have better social support networks, which can help them manage their health and cope with the challenges of CKD and ESRD.
This study also indicated that patients with higher education tend to be referred earlier for the treatment of end-stage renal disease (ESRD). This finding is consistent with a study conducted in India which found that patients with higher education were referred earlier than those with lower education levels [30]. Similarly, the studies conducted in Poland, Hungary, and Romania found that patients with higher education were more likely to receive early referrals for ESRD treatment [64]. The implications of these findings are significant, as early referral for ESRD treatment is associated with better patient outcomes and reduced healthcare costs. The reasons for the association of higher education with early referral are not entirely clear. Patients with higher education may be more likely to be aware of the symptoms and risk factors of ESRD, leading them to seek medical attention earlier. Additionally, healthcare providers may be more likely to refer patients with higher education levels due to better communication and understanding of the disease process. Overall, the findings from these studies suggested that efforts to increase awareness and education about ESRD may be beneficial in improving early referrals and patient outcomes. Healthcare providers should be aware of the potential for educational disparities in ESRD referrals and work to ensure that all patients receive appropriate and timely care [30, 65].
To our knowledge, this is the first study to be conducted in Jazan province to evaluate the baseline characteristics of hemodialysis patients and the rate of vascular access preparation. Another strong point in this study is the involvement of all governmental hemodialysis centers in Jazan, which allows for better evaluation and generalizability of study findings. Nonetheless, some notable limitations to our study should be discussed. The data has been recorded from patients' files and complimented with direct patients interviews due to a lack of inadequate data to cover the data instrument items. However, this hybrid approach to data collection has allowed better coverage of all study question variables. The practicing nephrologists may have to put an additional effort of documentations in order to improve hemodialysis patients’ outcomes and help the stakeholders to perform the necessary actions.
CONCLUSION
The prevalence of ESRD on hemodialysis has been shown to be higher in middle-aged male patients. Hypertension is the most implicated cause of ESRD in this cohort. AVF is less utilized as the preferred hemodialysis vascular access in Jazan region. The majority of study participants were referred late or even not referred. Early referral rates were significantly influenced by the educational level. Improvement of overall regional nephrology care is of paramount importance particularly for early referral for renal replacement therapy and arteriovenous fistula as the preferred vascular access in hemodialysis patients.
AUTHOR CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| CKD | = Chronic Kidney Disease |
| HTN | = Hypertension |
| DM | = Diabetes Mellitus |
| eGFR | = Estimated Glomerular Filtration Rate |
| RRT | = Renal Replacement Therapy |
| ESRD | = End-stage Renal Disease |
| HD | = Hemodialysis |
| SCA | = Sickle Cell Anemia |
| CGN | = Chronic Glomerulonephritis |
| SLE | = Systemic Lupus Erythematosus |
| KDIGO | = Kidney Disease Initiative Global Outcomes |
| MOH | = Ministry of Health |
| VA | = Vascular Access |
| AVG | = Arteriovenous Grafts |
| AVF | = Arteriovenous Fistula |
| CVCs | = Central Venous Catheters |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was reviewed and approved by the Research Ethics Committee-MOH in Jazan, Saudia Arabia Approval No.:22060; date:29 June 2022.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
For participants whose data were not available in the electronic system, informed consent was taken.


