All published articles of this journal are available on ScienceDirect.
Comparing the Effectiveness and Safety of Anterior Cervical Discectomy and Fusion with Four Different Fixation Systems: A Systematic Review and Network Meta-analysis
Abstract
Background:
Anterior cervical discectomy and fusion (ACDF) is the classic procedure for the treatment of degenerative cervical myelopathy (DCM). Cage with plate (CP), polyetheretherketone cage alone (PCA), ROI-C and Zero-P are the most widely used fixation systems in ACDF. However, there is insufficient evidence to determine the optimal system for ACDF.
Purpose:
A comprehensive analysis to show which of the CP, PCA, ROI-C and Zero-P after ACDF has the best clinical efficacy and the most reliable safety.
Methods:
We searched the Embase, Pubmed, and Cochrane library up to the date of February 13th, 2021. Studies included relevant randomized controlled trials (RCTs) and cohort studies with a comparison of different fixation systems among CP, PCA, ROI-C and Zero-P were identified.
Results:
We screened 43 trials eligible, including 3045 patients. No significant differences were found in the NDI score. PCA has shown a significantly less recovery of cervical lordosis than CP and Zero-P. For the non-fusion rate, PCA was significantly higher than CP. PCA had a significantly higher subsidence rate than CP and Zero-P, and ROI-C was also significantly higher than CP. For the incidence of complications, CP was significantly higher than the others. The surface under the cumulative ranking curves (SUCRA) for NDI score improvement was: SSC, PCA, and CP. ROI-C, Zero-P, PCA, and CP; for cervical lordosis recovery: CP, Zero-P, ROI-C, and PCA; for non-fusion rate: PCA, Zero-P, ROI-C, and CP; for subsidence rate: PCA, ROI-C, Zero-P, and CP; for complications: CP, PCA, ROI-C, and Zero-P.
Conclusion:
Despite the third-ranking spectrums of fusion rate, Zero-P still could be recommended for its second-ranking spectrums of the NDI score improvement efficacy, cervical lordosis recovery, and reduction of subsidence rate, with the least ranking of complications.
Registration:
The number of PROSPERO is CRD42021230735 (www.crd.york.ac.uk/PROSPERO).
1. INTRODUCTION
Smith and Cloward reported anterior cervical discectomy and fusion (ACDF) as the most classic procedure for the treatment of degenerative cervical myelopathy about 70 years ago [1-3]. Due to the convenience of nerve decompression and certain fusion via stable internal fixation and intervertebral bone grafting [4, 5], it was the most widely acceptable operation method to treat degenerative cervical spine disease by surgeons all around the world [6]. For a long period, the cage with plate (CP) has been recognised as the ‘golden’ standard approach for ventral internal fixation [7, 8]. Although largely with satisfactory efficacy, some complications, such as adjacent segment disease (ASD) and dysphagia, are inevitable [9, 10]. Therefore, considering the reliability, new fixation systems have been developed to reduce the risk of potential complications [11].
Alternatively, PCA has been investigated to improve the morbidity associated with conventional CP [12, 13]. Meanwhile, several inevitable complications, such as cage subsidence and cervical kyphosis, have been reported [14, 15]. To not only ensure the immediate postoperative stabilisation as CP without an anterior plate but also to minimise complications, especially dysphagia as PCA, ROI-C and Zero-P as stand-alone self-locking cage (SSC) system have been designed [16-19].
However, identifying the four most widely applied fixation systems is the best choice. Previous pairwise meta-analyses have only directly compared PCA with CP and SSC with CP [20-33], whereas studies comparing PCA and SSC are still lacking. Therefore, adequate evidence insufficiently ensured the optimal system for degenerative cervical spine disease. Network meta-analysis (NMA) has been developed to provide indirect results of more than two options based on indirect outcomes and a rank of all options [34]. Hence, an NMA was constructed to comprehensively analyse and rank the four fixation systems based on the neck disability index (NDI) score, subsidence, un-fusion, cervical lordosis and complications.
2. METHODS
Our study complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses and assessed the methodological quality of systematic review guidelines [20, 21].
2.1. Inclusion and Exclusion Criteria
2.1.1. Types of Studies
For the meta-analysis, we designed to properly include both RCTs and non-RCTs evaluating the effects and safety of CP, PCA, Zero-P and ROI-C applied during ACDF. For accessing the quality of the included literature, abstract-only papers and RCT protocols were excluded. Furthermore, meta-analysis, review articles, case reports, conference papers, cadaveric and animal research or unextractable data were all excluded.
2.1.2. Types of Participants
We included studies comprising adults (age ≥18 years) with ACDF. No restrictions on gender or race were established.
2.1.3. Types of Interventions
Studies aiming at any comparative CP, ROI-C, Zero-P and PCA during ACDF were included. At least two of four internal fixations were required in each study.
2.1.4. Types of Outcomes
Results included five main outcomes: NDI score, subsidence, un-fusion, cervical lordosis and complications.
2.1.5. Search Strategy
PubMed, Embase and the Cochrane Central Register of Controlled Trials were searched until June 31st, 2021. The following keywords were used to specifically search databases for anterior cervical discectomy and fusion, CP, PEEK cage, ROI-C, Zero-P and other additional words. The search strategy of Pubmed is listed in Appendix 1. Previous systematic reviews and meta-analyses of ACDF were reviewed to search for relevant trials. Only English publications were screened.
2.1.6. Study Selection
After combining identified results and removing duplications, two reviewers (HY and XL) independently reviewed the titles and abstracts of all studies retrieved during the search. During our study inclusion procedure, when institutions published duplicate studies, only the most complete or latest reports were included to minimize potential publication bias unless the population was definitely different according to the surgical levels or surgical periods. Besides, the full text was obtained and examined as necessary. Then, potentially relevant studies were selected following the eligibility criteria. If any disagreement occurred in one study, a third reviewer (YXD) was consulted.
2.1.7. Data Extraction and Quality Assessment
Two reviewers (HY and XL) extracted the basic information from included studies using a pre-designed extraction form. The extracted information was as follows: (1) study characteristics such as lead author, publication year, study design, study period and follow-up time; (2) demographic information: number of involved patients, percentage of male patients and age at operation; (3) surgical information (intervention and comparison); (4) outcome information: NDI score, subsidence number, un-fusion number, cervical lordosis and complications. If the SD of changes from the baseline cannot be acquired, SD was imputed using the method from the Cochrane Handbook. Then, the correlation coefficient values of 0.5 and 1 were also calculated for consistency.
2.1.8. Network Geometry
The network of five outcomes was presented as graphs. The size of the circle represented the number of patients, and the edge thickness represented the number of studies. The qualitative description of network geometry was described.
2.1.9. Risk of Bias within Individual Studies
The Newcastle-Ottawa Scale (NOS) [35] was used to assess the risk of bias of non-RCTs, whereas the Cochrane tool was used to assess the risk of bias of RCTs. XL and HY were independently evaluated. The grading difference was discussed, and a consensus was reached after a discussion. After calculating all meta-analyses, a summary of the findings table was established following the GRADE system [36].
2.1.10. Summary Measures
The NDI score improvement and cervical lordosis correction were individually measured as the mean difference (MD) with a 95% confidence interval (CI). Subsidence, un-fusion and complication rates were individually measured as odds ratio (OR) with 95% CI. Treatment ranking and the surface under the cumulative ranking curves (SUCRA) values were calculated.
2.1.11. Planned Analysis Methods
Outcomes with the same pairs of treatments were extracted. Direct evidence (pairwise meta-analysis) was analysed by a random-effects model. MD with 95% CI for the NDI score improvement and cervical lordosis correction as a continuous outcome. Moreover, OR with 95% CI for subsidence, un-fusion and complication rates as dichotomous outcomes were presented. Statistical heterogeneity was evaluated by the χ2 test and inconsistency (I2). STATA with Metan package (Version 15.0; STATA Corporation, College Station, TX) was used to calculate all outcomes.
Then, NMA was created within the Bayesian framework using the Markov Chain Monte Carlo algorithm in WinBUGS (Bayesian inference Using Gibbs Sampling for Windows, Version 1.4.3; Imperial College and MRC, UK) [37] with a random-effects model. The model was simulated on 3 Markov chains for 100,000 iterations after a burn-in of 50,000. A total of 10 iterations were applied as the thinning interval. The direct and indirect variances of convergence were evaluated using the Brooks–Gelman–Rubin method [38]. The potential scale reduction factor is close to or equivalent to 1, indicating the achievement of convergence [38]. NMA results were also presented as MD with 95% CI and OR with 95% CI. The rank of four fixation methods was calculated by WinBUGS, and results were inputted by STATA to generate SUCRA [39]. The SUCRA value was presented as 0% (the worst treatment) to 100% (the best treatment). Comparisons with NDI and cervical lordosis correction recorded pre-operatively are shown in a forest plot to assess the absolute therapeutic efficacy of all procedures.
2.2. Assessment of Inconsistency
2.2.1. Risk of Bias Across Studies
To measure the global inconsistency, consistency and inconsistency models were built, respectively. A reduction of >3 in the deviance information criterion (DIC) indicated inconsistency. The node-splitting method was used to evaluate the local model inconsistency [40]. A p-value of >0.05 indicated no inconsistency.
2.2.2. Sensitivity and Subgroup Analyses
In sensitivity analysis, SUCRA was recalculated after excluding low-quality studies. Moreover, the ranking of four internal fixations was compared with the previous ones. If no significant changes were observed, the results were robust.
Therefore, this study aimed to find whether some fixations were more suitable for two levels or more during ACDF. A subgroup analysis was evaluated. The mean surgical levels of ACDF were extracted from each study. Studies were grouped by ACDF with ≤2 or >2 levels. The covariate was represented as a single interaction term recommended by the UK’s National Institute for Health and Care Excellence [41].
3. RESULTS
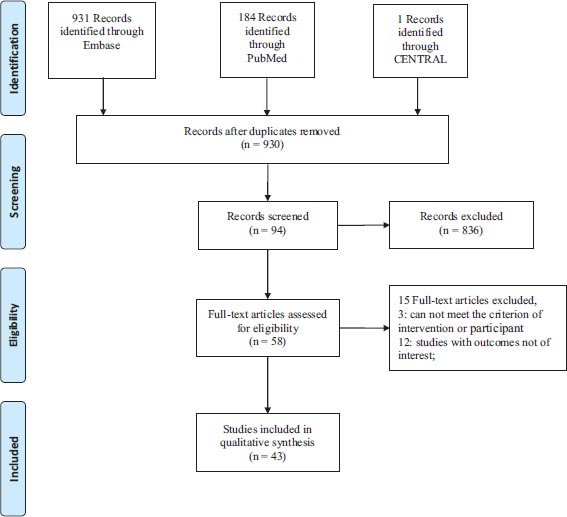
3.1. Documentation Retrieval
A total of 1116 potential titles were screened in the first search strategy, with 186 excluded due to duplications. Among the remaining 930 studies, 58 potentially qualified articles were acquired to check for eligibility after carefully screening titles and abstracts. With careful full-text reading, 15 studies were excluded due to the reasons shown in Fig. (1). Finally, 43 articles were included in our study [13, 19, 42-82].
3.2. Network Graphs
All comparison networks are shown in Fig. (2). The network included 1513 patients for NDI score, 2044 for cervical lordosis correction, 2087 for un-fusion rate, 1974 for subsidence rate and 2199 for complications.
3.3. Characteristics of the Included Trials
A total of 3045 patients were recorded. The network included 1513, 2044, 2087, 1974 and 2199 for NDI score, cervical lordosis correction, un-fusion rate, subsidence rate and complications, respectively. Six studies were RCT, 4 were prospective, and 33 were retrospective studies. We recorded the characteristics of all included studies in Table S1.
3.4. Risk of Bias and Quality Assessment
According to the NOS, Table S2 presents a quantification of the risk of bias assessment. A range of 7–9 stars was achieved by evaluating the NOS with an average score of 7.95, indicating that 38 studies were all of high quality (NOS score, ≥6). A total of 34 non-RCT studies reported the inclusion and exclusion criteria. However, selection bias was inevitable because the studies were not randomised.
Results of the risk of bias analysis of the included five RCTs generated using RevMan software are listed in Fig. S1. The generation of a random sequence was described in detail in two studies. Allocation concealment was mentioned in two studies. Performance bias is worst with only one study reported. The detection bias was described in detail in two studies. Thus, selection, performance and detection bias possibly led to bias.
Funnel plots evaluated the publication bias, and results indicated the absence of small-study effects for primary outcomes (Fig. 3).
Results of the GRADE evaluation of OPLL interventions are presented in Table S3. All reasons for downgrading and upgrading were labelled. As most of the trials were retrospective, grades were low and very low, respectively.
3.5. NDI Score Results
The results of the NDI score are shown in Table 1A. The lower-left triangle indicated pairwise meta-analysis, and the upper-right triangle indicated NMA. The shadows represented significant differences. The ROI-C showed slightly better NDI scores improvement than CP in pairwise meta-analysis [MD = −0.78, 95% CI: (−1.44, −0.11)]. Other than that, no other significant differences were found both in pairwise meta-analysis and NMA.
The forest plot Fig. (4) showed the absolute therapeutic efficacy of all procedures by comparing the NDI score. All treatments yielded a significant improvement in absolute therapeutic efficacy when compared with pre-operative values. Based on the results obtained from SUCRA, which comprised nearly 100% representing better effectiveness, ROI-C ranked best (74.2%), followed by Zero-P (58.9%), PCA (44.3%) and CP (22.5%), respectively (Fig. 5).
3.5.1. Results of Cervical Lordosis Correction
The results of cervical lordosis correction are shown in Table 1B. CP showed significantly better cervical lordosis correction than PCA both in pairwise meta-analysis [MD = 0.91, 95% CI: (0.10, 1.72)] and NMA [MD = 1.57, 95% CI: (0.35, 3.07)]. PCA did not significantly differ from Zero-P in NMA. Zero-P was better than PCA in pairwise meta-analysis [MD = 3.74, 95% CI: (0.76, 6.73)]. Other than that, no other significant differences were found.
The forest plot Fig. (4) showed the absolute cervical lordosis correction of all procedures by comparing NDI scores. All treatments yielded a significant improvement in absolute therapeutic efficacy when compared with pre-operative values. Based on results obtained from SUCRA, which comprises nearly 100% having a better cervical lordosis correction, CP ranked highest (92.3%), followed by Zero-P (59.6%), ROI-C (32.1%) and PCA (16.1%) (Fig. 5).
3.5.2. Results of Un-fusion Rate
Results of the un-fusion rate are shown in Table 1C. PCA showed a significantly higher un-fusion rate than CP both in pairwise meta-analysis [OR = 1.94, 95% CI: (1.12, 3.36)] and NMA [OR = 1.95, 95% CI: (1.13, 3.19)]. No other significant differences were found between them. Based on results obtained from SUCRA, PCA ranked to have the highest un-fusion rate (87.8%), followed by Zero-P (59.2%), ROI-C (38.1%) and CP (14.9%), respectively (Fig. 5).
3.5.3. Results of Subsidence Rate
The results of the subsidence rate are shown in Table 1D. PCA showed a significantly higher subsidence rate than CP and Zero-P both in pairwise meta-analysis [OR = 2.90, 95% CI: (2.13, 3.96); OR = 2.37, 95% CI: (1.02, 5.53), respectively] and NMA [OR = 3.03, 95% CI: (2.00, 4.38); OR = 2.52, 95% CI: (1.32, 4.42), respectively]. The ROI-C also showed a significantly higher subsidence rate than CP both in pairwise meta-analysis [OR = 2.13, 95% CI: (1.19, 3.81)] and NMA [OR = 2.35, 95% CI: (1.04, 4.69)]. No significant differences were found when comparing Zero-P with CP, Zero-P with ROI-C and PCA with ROI-C. Based on the results obtained from SUCRA, PCA had the highest subsidence rate (92.3%), followed by ROI-C (70.0%), Zero-P (30.3%) and CP (7.4%), respectively (Fig. 5).
3.5.4. Results of Complications
The results of the subsidence rate are shown in Table 1E. ROI-C and Zero-P showed a significantly lower incidence of complications than CP both in pairwise meta-analysis [OR = 0.33, 95% CI: (0.20, 0.56); OR = 0.26, 95% CI: (0.17, 0.40), respectively] and NMA [OR = 0.32, 95% CI: (0.16, 0.58); OR = 0.25, 95% CI: (0.13, 0.41), respectively]. PCA also showed a significantly lower incidence of complications than CP in NMA [OR = 0.51, 95% CI: (0.28, 0.85)], whereas no significant differences were found in the pairwise meta-analysis. Meanwhile, no significant differences were found when comparing Zero-P with ROI-C, Zero-P with PCA and PCA with ROI-C. Based on the results obtained from SUCRA, CP had the highest incidence of complications (99.8%), followed by PCA (61.9%), ROI-C (28.2%) and Zero-P (10.2%), respectively (Fig. 5).
Furthermore, the high pseudarthrosis rates (2.99%) should be considered in the PCA group. Notably, the high incidence of ASD should be more carefully considered when choosing PCA (3.55%) and CP (6.19%) groups. It should also be noted that all four groups were related to a higher dysphagia rate (Table 2).
3.6. Inconsistency Analysis
The results of inconsistency are listed in Table 3. For all outcomes, the difference in DIC between consistency and inconsistency was not >5. No local inconsistencies were detected (p-values, >.05).
3.6.1. Sensitivity and Subgroup Analysis
On excluding low-quality studies (Gerszten 2016) [42-48], the rank probabilities did not change. After systematically reviewing the indications of all procedures in the included studies, performing PCA would not be recommended with >2 levels. Therefore, we grouped the study based on two levels of surgical level definitions to perform subgroup analysis. Moreover, the results for the subgroup are presented in Table 3. No significant changes were observed between the two groups.
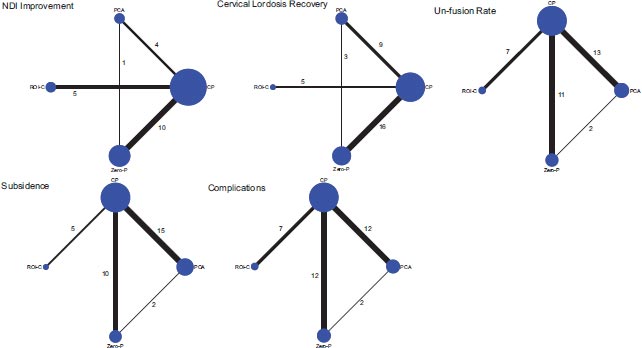
Note: The circle means the number of patients, and the edge thickness means the number of studies. CP, cage with plate; PCA, PEEK cage alone; NDI, Neck Disabilitv Index.
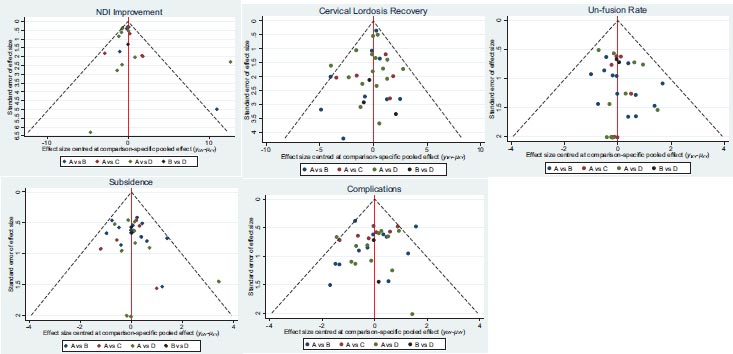
Note: The red full line represents the null hypothesis that the study-specific effect sizes do not differ from the respective comparison-specific pooled effect estimates. The two black dashed lines represent a 95% CI for the difference between study-specific effect sizes and comparisonspecific summary estimates. yixy is the noted effect size in study i that compares x with y. μxy is the comparison-specific summary estimate for x versus y. A = CP, B = PCA, C = ROI-C, D = Zero-P. CP, cage with plate; PCA, PEEK cage alone; NDI, Neck Disabilitv Index.
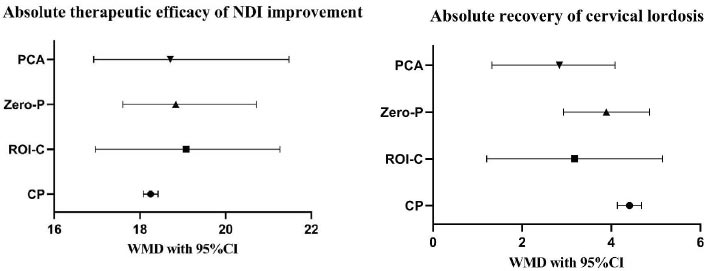
Note: CP, cage with plate; PCA, PEEK cage alone; NDI, Neck Disabilitv Index.
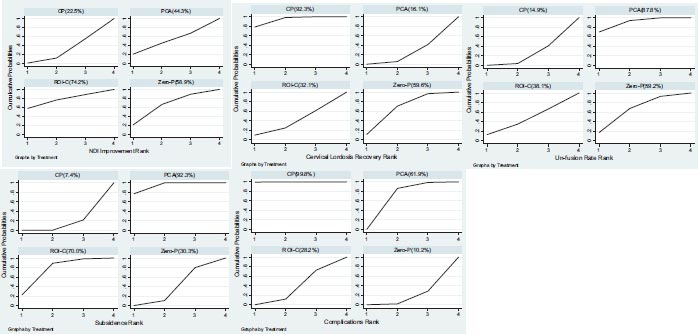
The cumulative rank probabilities of the three treatments were shown as the area under the curve. A larger area represents a better cumulative rank probability and a higher incidence. CP, cage with plate; PCA, PEEK cage alone; NDI, Neck Disability Index.
| CP | -0.83 (-3.01,1.28) | -0.59 (-2.47,0.63) | -0.46 (-3.23, 1.34) |
|---|---|---|---|
| N=5, -0.78 (-1.44, -0.11) | ROI-C | 0.25 (-2.65,2.61) | 0.37 (-3.21, 3.05) |
| N=10, -0.74 (-1.85, 0.37) | - | Zero-P | 0.13 (-2.57, 2.51) |
| N=4, 0.14 (-0.74, 1.02) | - | N=1, -1.80 (-4.35,0.75) | PCA |
| CP | 1.23 (-0.71, 3.19) | 0.52 (-0.43, 1.44) | 1.57 (0.35, 3.07) |
|---|---|---|---|
| N=5, 1.24 (-0.69, 3.18) | ROI-C | -0.71 (-2.88, 1.4) | 0.34 (-1.93, 2.79) |
| N=16, 0.50 (-0.05, 1.05) | - | Zero-P | 1.05 (-0.41, 2.79) |
| N=9, 0.91 (0.10, 1.72) | - | N=3, 3.74 (0.76, 6.73) | PCA |
| CP | 1.26 (0.55, 2.50) | 1.49 (0.84, 2.48) | 1.95 (1.13, 3.19) |
|---|---|---|---|
| N=7,1.16 (0.59, 2.29) | ROI-C | 1.37 (0.48, 3.07) | 1.79 (0.64, 3.96) |
| N=11,1.42 (0.83, 2.45) | - | Zero-P | 1.39 (0.68, 2.56) |
| N=13, 1.94 (1.12, 3.36) | - | N=2, 1.22 (0.45, 3.28) | PCA |
| CP | 2.35 (1.04,4.69) | 1.28 (0.72,2.11) | 3.03 (2.00,4.38) |
|---|---|---|---|
| N=5,2.13 (1.19,3.80) | ROI-C | 0.63 (0.23,1.42) | 1.49 (0.57,3.18) |
| N=10,1.10 (0.71,1.70) | - | Zero-P | 2.52 (1.32,4.42) |
| N=15,2.90 (2.13,3.96) | - | N=2,2.37 (1.02,5.53) | PCA |
Table 1E.
| CP | 0.32 (0.16, 0.58) | 0.25 (0.13, 0.41) | 0.51 (0.28, 0.85) |
|---|---|---|---|
| N=7,0.33 (0.20, 0.56) | ROI-C | 0.86 (0.33, 1.85) | 1.78 (0.69, 3.79) |
| N=12,0.26 (0.17, 0.40) | - | Zero-P | 2.24 (0.99, 4.39) |
| N=12,0.55 (0.30, 1.01) | - | N=2, 1.16 (0.33, 4.12) | PCA |
3.7. Meta-regression
With meta-regression, no statistically significant difference in DIC was found when considering the sample size of the study (Table 3). These data indicate that the sample size was not associated with the therapeutic effect.
4. DISCUSSION
4.1. Main Results
To the best of our knowledge, this is the first comprehensive and integrated NMA to pool data focusing on NDI score improvement, cervical lordosis correction, un-fusion rate, subsidence rate and complication incidences of four widely applied fixation systems: PCA, ROI-C, Zero-P and CP in ACDF; this information can be used to help surgeons choose the optimal fixation system for their actual situations. The key findings of this systematic review and NMA show that (1) all of them have a significant effect in the NDI score improvement without significant differences; (2) a trend of cervical lordosis correction has been observed, whereas PCA shows lesser correction than CP and Zero-P; (3) PCA has a significantly higher un-fusion rate than CP, whereas no significant difference is found among others; 4) PCA shows a significantly higher subsidence rate than CP and Zero-P, and ROI-C is also significantly higher than CP, whereas no significant difference is observed between Zero-P and CP, or ROI-C; 5) CP has the highest incidence of complications, whereas no significant difference is found among others; and 6) the rank for NDI score improvement is as follows: ROI-C, Zero-P, PCA and CP; CP, Zero-P, ROI-C and PCA for cervical lordosis correction; PCA, Zero-P, ROI-C and CP for un-fusion rate; PCA, ROI-C, Zero-P and CP for subsidence rate; and CP, PCA, ROI-C and Zero-P for incidence of complications.
4.2. Main Findings and Interpretation based on Previous Studies
Regarding the clinical outcome measurements, the NDI score is an effective indicator to evaluate the patient’s functional recovery after ACDF83. Our pooled data of absolute therapeutic efficacy shows that all of them have a significantly improved NDI score, indicating that all techniques could have sufficient decompression and nerve improvement. By directly comparing ROI-C and CP shows a slight statistical difference, but the NMA shows no significant difference between them. Previous head-to-head meta-analyses and systematic reviews have been performed to deal with PCA versus CP and SSC versus CP [20-33]. Almost all studies concluded no strong evidence to support which of the three fixation systems is the best to improve NDI in ACDF. Although SSC was subdivided into ROI-C and Zero-P groups, there is no dispute that our findings are consistent with those of previous studies. Hence, no definite conclusions can be drawn based on the superiority of one fixation over the other in functional outcomes. Nevertheless, the subtle ranking among them is still distinguished via our comprehensive analysis.
| Complication | No. (%) | |||
|---|---|---|---|---|
| CP (N = 1083) | Zero-P (N = 397) | ROI-C (N = 217) | PCA (N = 535) | |
| CSF leakage | 8 (0.74) | 1 (0.25) | 6 (2.76) | 1 (0.19) |
| Implant dislocation | 19 (1.75) | 2 (0.50) | 0 | 7 (1.31) |
| Axial symptoms | 4 (0.37) | 0 | 1 (0.46) | 1 (0.19) |
| Pseudarthrosis | 8 (0.74) | 1 (0.25) | 0 | 16 (2.99) |
| Sore throat | 4 (0.37) | 0 | 2 (0.92) | 0 |
| Hematoma | 3 (0.28) | 0 | 0 | 1 (0.19) |
| Hoarseness | 15 (1.39) | 3 (0.76) | 1 (0.46) | 5 (0.93) |
| Infections | 3 (0.28) | 1 (0.25) | 1 (0.46) | 1 (0.19) |
| Neurological deterioration | 5 (0.46) | 1 (0.27) | 0 | 2 (0.37) |
| Progressive kyphosis | 2 (0.19) | 0 | 0 | 6 (1.12) |
| ASD | 67 (6.19) | 2 (0.50) | 4 (1.84) | 19 (3.55) |
| - | CP (N = 1187) | Zero-P (N = 505) | ROI-C (N = 217) | PCA (N = 567) |
| Dysphagia | 246 (20.72) | 66 (13.07) | 44 (20.28) | 36 (6.35) |
| - | NDI Improvement | Cervical Lordosis Correction | Un-fusion Rate | Subsidence Rate | Complications | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Local inconsistency | Comparison | p.value | Comparison | p.value | Comparison | p.value | Comparison | p.value | Comparison | p.value |
| CP vs Zero-P | 0.284 | CP vs Zero-P | 0.405 | CP vs Zero-P | 0.960 | Zero-P vs PCA | 0.917 | CP vs Zero-P | 0.472 | |
| CP vs PCA | 0.269 | CP vs PCA | 0.444 | CP vs PCA | 0.688 | CP vs PCA | 0.577 | |||
| Zero-P vs PCA | 0.276 | Zero-P vs PCA | 0.042 | Zero-P vs PCA | 0.902 | Zero-P vs PCA | 0.422 | |||
| DIC for global inconsistency | Consistency model | Inconsistency model | Consistency model | Inconsistency model | Consistency model | Inconsistency model | Consistency model | Inconsistency model | Consistency model | Inconsistency model |
| 90.82 | 91.04 | 96.333 | 97.558 | 74.367 | 76.321 | 96.822 | 96.757 | 104.630 | 105.672 | |
| DIC for meta-regression | without the covariate | with the covariate | without the covariate | with the covariate | without the covariate | with the covariate | without the covariate | with the covariate | without the covariate | with the covariate |
| 147.386 | 144.581 | 234.208 | 234.556 | 243.012 | 244.745 | 286.158 | 286.849 | 306.858 | 307.964 | |
| Meta-regression coefficient | 0.003613(-0.04028, 0.05509) | 0.01705(-0.01004, 0.04121) | -0.001549(-0.009446, 0.006316) | 0.002542(-0.003351, 0.008574) | -0.0003938(-0.0142, 0.01378) | |||||
| Subgroup analysis coefficient | 0.04339(-2.863, 3.042) | 0.2568(-1.159, 1.76) | 0.3647(-0.4867, -0.4867) | -0.5404(-1.168, 0.06011) | -0.06611(-0.8149, 0.683) | |||||
One of the main recognised goals of ACDF is to reconstruct and correct the cervical lordosis angle [83, 84]. Despite the encouraging findings that all have a trend of cervical lordosis correction, PCA is still associated with a poorer ability to restore and preserve cervical lordosis than others. CP has been widely accepted as the best global cervical lordosis correction effect, as the plate curve can reconstruct cervical sequencing and gain a stable fixation [28]. This conclusion, which is in line with biomechanic expectations, has been further confirmed in our study. Moreover, our results indicate that all CP, ROI-C and Zero-P have a similar ability to restore and preserve cervical lordosis. This finding is also consistent with those of previous meta-analyses and systematic reviews [20, 21, 23, 25-33]. Interestingly, a previous individual study and two meta-analyses have hypothesised that loss of cervical lordosis may be a main theoretical risk factor for ASD [20, 29, 85]. However, the results of our systematic analysis may result in a different view. The ASD rate in PCA is associated with approximately twofold less than CP (3.55% vs. 6.19%), indicating that rigid fixation with plates is probably the most important risk factor for ASD.
Unfusion can lead to immediate failure of the ACDF procedure and may result in serious complications [86]. Our results demonstrate that PCA has the most common un-fusion rate. With different fixation systems in ACDF, fusion regularly occurs at a higher rate due to rigidity [28]. Our systematic review data show that the pseudarthrosis rate in PCA is associated with approximately fourfold higher than CP, which further suggests that rigid fixation appears to mitigate concerns for pseudarthrosis. Therefore, our pooled data of un-fusion corresponds with what is expected from a biomechanical point of view. We also revealed a comparable un-fusion rate among CP, ROI-C and Zero-P. This result is also consistent with those of the previous meta-analyses [20, 21, 25, 29, 31-33].
One of the major concerns of ACDF is reducing the subsidence rate. Our pooled results demonstrate that PCA and ROI-C are both associated with a higher incidence of subsidence than CP. Several studies have reported that the use of plates can reduce the subsidence rate after ACDF [28, 50, 87]. This is well understood as more stress concentration in PCA and ROI-C, corresponding with expectations from a biomechanical perspective. Besides, Zero-P could also achieve comparable stability to reduce the incidence of subsidence to that of CP for ACDF. However, we must recognise that, as noted previously, no one standardised definition of ‘subsidence’ has been established. This unavoidable flaw seriously weakens our statistical strength of discoveries. Therefore, how well the subsidence rate correlates with clinical significance in this study remains to be elucidated. Efforts to report transparent and consistent standards in the future are strongly encouraged to improve validity.
Surgery-related complications are considered a crucial factor in deciding on a surgical procedure. Our pooled data suggest that CP has the highest complication rate. Remarkably, almost all previous meta-analyses only statistically analysed the incidence of dysphagia [20, 21, 23, 25-33]. Our results indicated that the incidence of dysphagia, kyphosis and ASD was closely associated with the choice of the type of internal fixation device. Undoubtedly, previous studies have concluded that the incidence of dysphagia is significantly higher in ACDF with a plate than that without a plate [10, 23]. The most likely reason for this is that the anterior plate after ACDF may directly compress and irritate the oesophagus and the surrounding soft tissues [9, 10, 88, 89]. Furthermore, intraoperative placements of the plate require more retraction of the oesophagus, which may be another reason for the high incidence of dysphagia [90]. Rigorous fixation should be compensated for the hypermobility of the adjacent segment after fusion [91]. This may be one of the major sources of developing ASD in PCA. In choosing the CA, stand-alone cages have issues of subsidence and local kyphosis at the index level [92]. Kyphosis at the index level may aggravate the degenerative changes in adjacent levels [93]. Considering that dysphagia accounts for a large proportion of complications, a consistent conclusion of total complications can be reached. More importantly, considering the high incidence of ASD in CP (6.35%) and PCA (3.55%), they should be carefully deliberated before the selection. Therefore, our study more comprehensively synthesises all existing evidence to provide simultaneous information regarding the rank of these four fixation systems.
5. LIMITATIONS
However, like many other meta-analyses, this study has some limitations. First, publication bias was inevitable for our meta-analysis, only including English publications. Second, a small proportion of the included studies were RCTs. Therefore, more RCTs would be needed for effectiveness and safety. Finally, different treatment centres had various surgical indications and technologies, which could be an essential heterogeneity source and thus making it challenging to compare the efficacy and complication of different surgeries. Nevertheless, given the high quality of the included studies, the results of our comparison are sufficiently convincing.
CONCLUSION
In conclusion, despite the second-ranking spectrums of the un-fusion rate, Zero-P could still be recommended for its second-ranking spectrums of the NDI score improvement efficacy, cervical lordosis correction and reduction of subsidence rate, with the least ranking of complications. Notably, the high incidence of ASD should be carefully considered before choosing CP and PCA. We would like to emphasise that this recommendation is based on low evidence as most of the available trials were retrospective. Therefore, well-designed RCTs are needed to obtain robust results to make any practice recommendations.
LIST OF ABBREVIATIONS
| CP | = Cage With Plate |
| PCA | = Polyether Ether Ketone Cage Alone |
| SSC | = Self-locking Cage |
| ASD | = Adjacent Segment Disease |
| ACDF | = Anterior Cervical Discectomy And Fusion |
| RCTs | = Randomised Controlled Trials |
| SUCRA | = Surface Under The Cumulative Ranking Curves |
| NMA | = Network Meta-analysis |
| NDI | = Neck Disability Index |
| PRISMA | = Preferred Reporting Items for Systematic Reviews and NMA |
| NOS | = Newcastle-Ottawa Scale |
| PSRF | = Potential Scale Reduction Factor |
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analysed during this study are included in this published article.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
FUNDING
The authors gratefully acknowledge the financial support from the National Major Scientific and Technological Special Project for the ‘National New Drug Innovation Program’ during the Thirteenth Five-Year Plan Period (2017ZX0 9304003) and the Guangzhou Municipal Science and Technology Project (202102080222).
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.
Supplementary material is available on the publisher’s website along with the published article.
| No. | Query |
|---|---|
| #11 | #9 and #10 |
| #10 | “titanium”[Title/Abstract] OR “polyetheretherketone”[Title/Abstract] OR “PEEK”[Title/Abstract] OR “zero-profile”[Title/Abstract] OR “zero-profile”[Title/Abstract] OR “zero-p”[Title/Abstract] OR “zero-p”[Title/Abstract] OR “anchored cage”[Title/Abstract] OR “anchored spacer”[Title/Abstract] OR “stand-alone”[Title/Abstract] OR “stand-alone”[Title/Abstract] OR “self-locking”[Title/Abstract] OR “plate”[Title/Abstract] OR “ROI-C”[Title/Abstract] OR “bridge-type”[Title/Abstract] OR “region-of-interest”[Title/Abstract] |
| #9 | #1 AND #8 |
| #8 | #2 AND #6 AND #7 |
| #7 | fusion[Title/Abstract] |
| #6 | #3 OR #4 OR #5 |
| #5 | discectomies[Title/Abstract] |
| #4 | microdiscectomy[Title/Abstract] |
| #3 | discectomy[Title/Abstract] |
| #2 | anterior[Title/Abstract]) AND (cervical[Title/Abstract] |
| #1 | ACDF[Title/Abstract] |


