All published articles of this journal are available on ScienceDirect.
LETTER TO THE EDITOR Haemophagocytosis in a Patient with Diffuse Large B Cell Lymphoma
DEAR EDITOR,
We report a case of a bone marrow biopsy specimen of a patient with history of weakness and bone pains since approximately three months. Past history was significant for blood and blood product transfusion. Examination findings revealed pallor with bilateral cervical and axillary-lymphadenopathy. He had left sided facial swelling. Biopsy of facial mass was consistent with Diffuse Large B Cell Non-Hodgkin’s Lymphoma. He was advised for bone marrow examination as part of staging. Complete blood counts performed with bone marrow showed Hb: 9.6 gm/dl, Hct: 29.0 %, MCV: 87.9 Fl, MCH: 29.1 PG, WBC: 14.4 x109/L, ANC: 9.9 x 109/L and Platelets: 109 x 109/L. Peripheral blood film showed dimorphic blood picture with anisocytosis, poikilocytosis, dysplastic neutrophils, occasional metamyelocytes and few large platelets. Bone marrow aspirate was a cellular specimen showing numerous histiocytes and prominent areas of haemophagocytosis with a few showing panphagocytosis. Bone trephine showed normal cellularity for age with prominent increase in histiocytes. Although there was no evidence of involvement of bone marrow with underlying lymphoma in the sections examined, the panphagocytosis in the bone marrow was probably related to the underlying lymphoma. Malignant histiocytosis was first described by Rappaport as asystemic, progressive, invasive proliferation of morphologically atypical histiocytes and their precursors [1]. More appropriately, now it is viewed as a syndrome that can result from a variety of hematological malignancies [2]. Haemophagocytosis in bone marrow aspirate has been reported previously. Janka et al. in 1998 reported hemophagocytic syndrome associated with DLBCL exclusively in patients from Asian countries [3]. Takeshita M et al. [4] reported a series of 19 patients with malignant histiocytosis and/or malignant lymphoma (ML) with concurrent hemophagocytic syndrome. Two of the patients had an underlying B-cell lymphoma. Erythrophagocytosis was more profound in this series. Fig. (1A-C) is showing prominent haemophagocytosis.
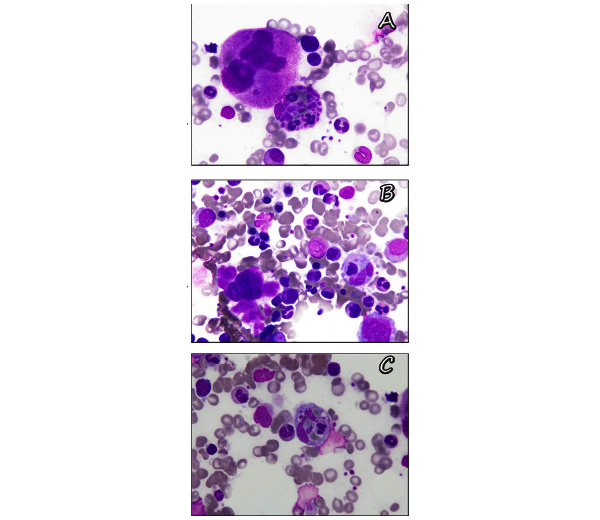
(A-C) Showing areas with panhaemophagocytosis.
AUTHORS CONTRIBUTION
Izza Hussain: took pictures, drafted manuscript.
Natasha Ali: drafted manuscript, critically reviewed the manuscript and submitted it.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
Declared none.


